Proposal for an Anatomic Guide in Cortical Bone Window Technique for Endodontic Microsurgery: A Case Report
June 12, 2024
J Endod Microsurg. 2024; 3: 100017.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE (AMA Referencing)
Castillo GA, Restrepo-Méndez SA, Gustin MF, Zamora IX. Proposal for an anatomic guide in cortical bone window technique for endodontic microsurgery: a case report. J Endod Microsurg. 2024;3:100017. https://doi.org/10.23999/j.jem.2024.3.4
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2024U000228/
. ABSTRACT IN UKRAINIAN (PDF). ABSTRACT IN SPANISH.
This case report describes a novel design for an anatomical guide used in endodontic microsurgery (EM) with the cortical bone window technique. A 60-year-old female patient presented with persistent pain and a radiographic periapical lesion associated with tooth #36 (i.e., lower left first molar). Following a diagnosis of symptomatic apical periodontitis, a treatment plan involving guided EM with static navigation was implemented. Cone-beam computed tomography (CBCT) data was segmented to create a stereolithographic (STL) file of the tooth. This file was aligned and 3D-printed with a biocompatible resin to create a customized anatomical guide. The guide facilitated a precise osteotomy, accurate apex localization, and conservative flap management during surgery. The surgical procedure was completed successfully, with minimal complications. Follow-up CBCT one month later demonstrated excellent adaptation of the bone fragment and apical seal. Using 3D imaging and a customized anatomical guide in EM demonstrates promising outcomes for treating complex cases. The proposed design offers advantages by eliminating the need for guide tubes and facilitating conservative flap management. Further clinical studies are recommended to validate the long-term efficacy of this technique.
KEYWORDS
Bone window; cone beam computed tomography; endodontic microsurgery; osteotomy; piezoelectric surgery
INTRODUCTION
Endodontic microsurgery (EM) is a surgical procedure to treat persistent periapical disease. This involves removing infected and affected tissue surrounding the root tip (periapical area) when previous non-surgical root canal treatment (endodontic therapy) or retreatment has failed [1]. The success rate of EM is currently around 94%. This high success rate can be attributed to various factors, such as the use of cone-beam computed tomography (CBCT), the operative microscope, the preparation of the root-end cavities with the ultrasonic devices, and the development of more biocompatible root-end filling materials, among other advancements [2]. However, this success rate can be reduced for several reasons, including the tooth's position in the mouth [3]. This is why lower molars can have lower success rates compared to teeth in other positions [4]. This is attributed to the difficulty of locating the root apices due to the thickness of the cortical bonhge of the vestibular wall and impediments in access by different anatomical structures, including the inferior alveolar nerve or the mental foramen [4].
For this reason, using three-dimensional (3D) computer-aided design/computer-aided manufacturing (CAD/CAM) guides has recently become common, optimizing the size of osteotomies, and minimizing the possibility of deviation according to the digitally established surgical planning [5, 6]. These guides, despite demonstrating great advantages, have some limitations. Antal et al. (2019) reported the difficulty in taking impressions and scanning in shallow vestibules, the positioning of the guide, and access of instruments due to the size of the mouth of some patients and the impossibility in some cases of performing apical cuts without angulation, situations that can affect the prognosis of the surgery [7].
In this case report, we present a design of an anatomical guide for endodontic microsurgery by use of the cortical bone window technique in a very precise way from the patient's tomography, digital segmentation, and 3D printing.
CASE REPORT
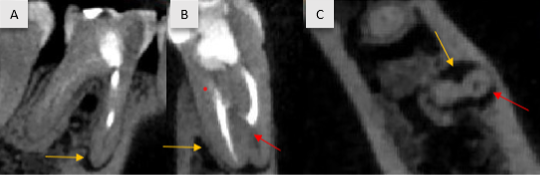
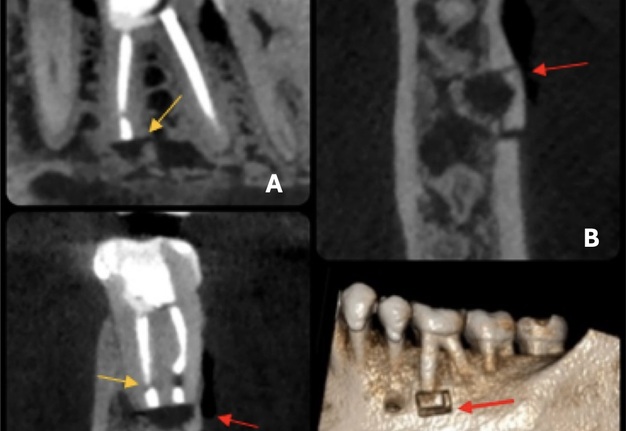
A 60-year-old female patient with no significant medical history was referred for evaluation and treatment of tooth #36 (i.e., lower left first molar) due to a history of pain when chewing. Dental history included endodontic treatment and retreatment performed approximately 6 months ago and persistent periapical lesion. On clinical examination, revealed an adapted occlusal restoration, ≤2 mm of periodontal probing, and painful on vertical percussion. Radiographically, previous endodontic treatment is observed, the mesiobuccal canal is underfilled with apparent transportation in the apical third of the root. Α hypodense area in the mesial root is also observed and the buccal cortical bone is intact (Fig 1). Based on the above findings, a diagnosis of previous endodontic treatment and symptomatic apical periodontitis was established. The treatment plan involved guided EM with static navigation, which the patient accepted through informed consent.
FIGURE 1. Preoperative cone-beam computed tomography of the tooth #36 (i.e., lower left first molar): (A) sagittal, (B) coronal, and (C) axial planes. The yellow arrow shows the periapical lesion, and the red arrow shows the mesiobuccal canal is underfilled with apparent transportation in the apical third. An intact thickness of vestibular cortical bone is present.
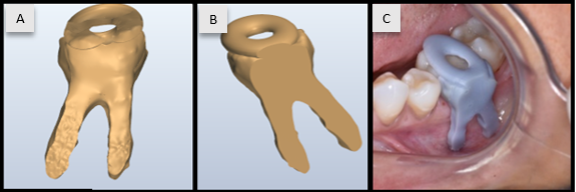
The Digital Imaging and Communications in Medicine (DICOM) files of CBCT (Myray Hyperion X9 Tomograph, Imola, Italy) voxel size 75 μm, field of view 60x40mm- were imported into the Mimics software (Materialise NV, Leuven, Belgium) and then the segmentation for the tooth #36 was performed. The stereolithography (STL) file of the tooth was aligned and projected toward the buccal cortical bone plate. Subsequently, a Boolean was added to the occlusal anatomy of the tooth to reproduce the digital position at the time of surgery. This stereolithographic file was printed on a 3D Creality printer (HALOT-MAGE, Shenzhen, China) with a biocompatible resin, Die, and Model 2 from SprintRay (Los Angeles, California, USA) (Fig 2).
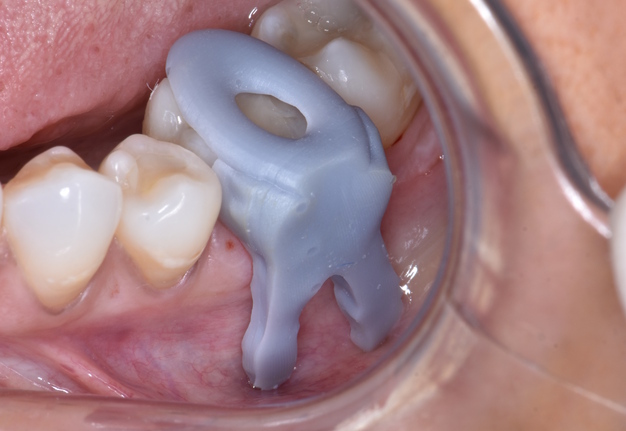
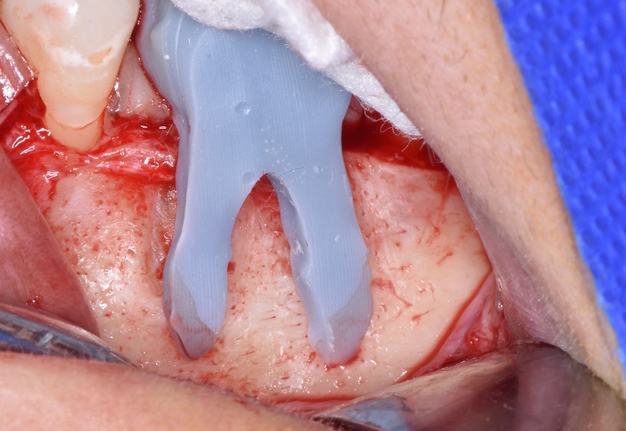
Before the procedure (Fig 3), the patient rinsed with 0.12% chlorhexidine (Clorhexol, Farpag S.A.S., Bogotá, Colombia) for 1 minute. For local anesthesia, 3 cartridges of 2% lidocaine with 1:80,000 epinephrine (New Stetic S.A., Guarne, Colombia) were used: 2 cartridges for inferior alveolar nerve block and 1 cartridge to anesthetize the mental nerve. A rectangular full thickness intrasulcular flap was raised from the mesial aspect of tooth #35 to the distal aspect of tooth #37. After raising the flap, the adaptation of the guide was checked, and the patient was asked to bite on a gauze to secure the printed device (Fig 3B). Next, with the aid of magnification (operative microscope Zumax OMS 2350, Zumax Medical Co., Ltd., Suzhou New District, China), the US3 tip (Ultrasurgic touch, Woodpecker Medical Instrument Co. LTD, Guilin, Guangxi, China) of the Surgic Touch piezoelectric system (Woodpecker Ultrasurgic Touch unit, Guilin Woodpecker Medical Instrument Co. LTD, Guilin, Guangxi, China) was used (Fig 3C, D) to create a 5mm x 3mm surgical bone window using the apex of the anatomical guide as a reference. After lightly marking the outline, the printed device was removed, and the cortical bone was completely cut by applying more pressure to the bone under ample abundant irrigation with saline solution and 7 high-power settings. The bone fragment was removed and placed in a saline solution until the end of the surgical procedure.
The exposed root was examined (Fig 3E), and the accuracy of the guide was verified. An apicoectomy (3 mm) was performed using the same tip, and the apex was removed along with the lesion. The cavity was irrigated with saline solution, and hemostasis was achieved with sterile cotton pellets soaked with adrenaline 1mg/ml solution injectable (B.Braun Surgical, Medellín, Colombia) placed at the bottom of the osteotomy. The root-end preparation was carried out with EM ultrasonic diamond tip a tip (E30LD, NSK/Nakanishi Inc, Tochini, Japan) after a detailed observation with methylene blue and magnification (Fig 3F).
Retrograde obturation was performed with Bio-C Repair bioceramic reparative material (Angelus Indústria de Produtos Odontológicos S/A, Londrina, Brazil). After inspecting the seal, CollaTape® collagen wound dressing (Zimplant & CIA S.A.S, Bogotá, Colombia) was placed in the bone crypt, and the cortical window was repositioned (Fig 3G). The same collagen wound dressing was used to stabilize the bone fragment before repositioning the flap. Figure 4 demonstrate sequence of the surgical steps. Suturing was done with Dafilon 5-0 monofilament suture (B. Braun Surgical S.A., Rubi, Spain). Written recommendations were given to the patient, and she was prescribed Amoxil (GlaxoSmithKline [GSK], London, England) capsules 500 mg #15 every 8 hours and Anexia (Tecnoquímicas S.A., Cali, Colombia) tablets 120mg #5 daily. The patient returned after 7 days for suture removal without any postoperative complications. A CBCT was performed one month later, which showed excellent adaptation of the bone fragment and apical seal (Fig 5).
FIGURE 3A. Clinical sequence of the anatomic guide in cortical bone window technique on tooth #36. (A) Pre- and (B) intraoperative positioning of the guide. (C, D) Piezoelectric cutting with the surgical guide in position. (E) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (F) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (G) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
FIGURE 3B. Clinical sequence of the anatomic guide in cortical bone window technique on tooth #36. (A) Pre- and (B) intraoperative positioning of the guide. (C, D) Piezoelectric cutting with the surgical guide in position. (E) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (F) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (G) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
FIGURE 3C. Clinical sequence of the anatomic guide in cortical bone window technique on tooth #36. (A) Pre- and (B) intraoperative positioning of the guide. (C, D) Piezoelectric cutting with the surgical guide in position. (E) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (F) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (G) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
FIGURE 3D. Clinical sequence of the anatomic guide in cortical bone window technique on tooth #36. (A) Pre- and (B) intraoperative positioning of the guide. (C, D) Piezoelectric cutting with the surgical guide in position. (E) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (F) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (G) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
FIGURE 3E. Clinical sequence of the anatomic guide in cortical bone window technique on tooth #36. (A) Pre- and (B) intraoperative positioning of the guide. (C, D) Piezoelectric cutting with the surgical guide in position. (E) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (F) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (G) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
FIGURE 3F. Clinical sequence of the anatomic guide in cortical bone window technique on tooth #36. (A) Pre- and (B) intraoperative positioning of the guide. (C, D) Piezoelectric cutting with the surgical guide in position. (E) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (F) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (G) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
FIGURE 3G. Clinical sequence of the anatomic guide in cortical bone window technique on tooth #36. (A) Pre- and (B) intraoperative positioning of the guide. (C, D) Piezoelectric cutting with the surgical guide in position. (E) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (F) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (G) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
FIGURE 4. (A) Virtual planning and (B-H) clinical sequence of the anatomic guide in cortical bone window techniqueon tooth #36. (B) Pre- and (C) intraoperative positioning of the guide. (D, E) Piezoelectric cutting with the surgical guide in position. (F) the exposed root was examined, and apicectomy (3 mm) was performed using the same tip, (G) retrograde obturation was performed with BioC repair cement (Angelus, Londrina, Brazil). (H) CollaTape® collagen membrane (Zimplant, Bogotá, Colombia) was placed in the cavity, and the cortical bone fragment was repositioned.
DISCUSSION
The current trend for resolving complex cases in endodontic clinical practice is based on the use of 3D images for the visualization of anatomical structures, diagnosis, and precise planning of surgical treatments, such as the specific case of designing guides for complex procedures, whose characteristics potentially allow reducing the surgical intervention time and postoperative complications [8, 9].
The use of these surgical guides with the management of piezo-surgery allows for precise osteotomy with immediate apex location, improving visibility, and reducing bleeding, since they provide a precise and safe approach through the selective cutting of mineralized tissues such as bone and the preservation of soft tissues such as blood vessels, nerves, and mucous membranes. Improving postoperative effects during the healing time for the patient [6, 10-14].
Multiple designs and different software for the manufacturing of guides have been widely documented [15, 16]. In the technique presented, a compact and personalized design is involved, without the help of guide tubes that allows obtaining the outline of the tooth to be treated, superimposed on itself and soft tissues or the same underlying intact bone, facilitating the lifting of a conservative flap and without the need to perform an aggressive retraction of the mouth, also achieving the precise location of the root apex.
Considering the limitations of this technical report, the result of the guided surgical approach presented above is promising; it makes it possible to perform a guided osteotomy, apex location, and resection of the root apex according to digital planning, of course, considering and respecting the recommended guidelines for contemporary endodontic surgical procedures. To confirm the reliability of this method in the future, it is recommended to carry out clinical studies to test and confirm its viability and precision.
CONCLUSION
The utilization of 3D imaging and customized anatomical guides in EM presented in this case report demonstrates promising outcomes for treating complex cases. The guided approach facilitated precise osteotomy, accurate apex localization, and conservative flap management, potentially reducing surgical time and postoperative complications. Further clinical studies are recommended to validate the reliability and efficacy of this technique across a larger patient population.
AUTHOR CONTRIBUTIONS
Conceptualization: Gustavo A. Castillo, Martin F. Gustin. Data acquisition: Gustavo A. Castillo, Silvia A. Restrepo Mendez, Martin F. Gustin, Ingrid X. Zamora. Data analysis or interpretation: Gustavo A. Castillo, Silvia A. Restrepo Mendez, Martin F. Gustin, Ingrid X. Zamora. Drafting of the manuscript: Gustavo A. Castillo, Silvia A. Restrepo Mendez, Martin F. Gustin, Ingrid X. Zamora. Critical revision of the manuscript: Gustavo A. Castillo, Ingrid X. Zamora. Approval of the final version of the manuscript: all authors.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ORCID
Gustavo A. Castillo: https://orcid.org/0009-0002-0534-9941
Silvia A. Restrepo-Méndez: https://orcid.org/0009-0005-6021-2229
Martin F. Gustin: https://orcid.org/0000-0002-9547-2988
Ingrid X. Zamora: https://orcid.org/0000-0002-9287-1414
REFERENCES (16)
-
Chong BS, Rhodes JS. Endodontic surgery. J Br Dent. 2014;216:281-290. https://doi.org/10.1038/sj.bdj.2014.220
-
Kohli MR, Berenji H, Setzer FC, et al. Outcome of endodontic surgery: a meta-analysis of the literature-part 3: comparison of endodontic microsurgical techniques with 2 different root-end filling materials. J Endod. 2018;44(6):923-931. https://doi.org/10.1016/j.joen.2018.02.021
-
Kim U, Kim S, Kim E. The application of "bone window technique" using piezoelectric saws and a CAD/CAM-guided surgical stent in endodontic microsurgery on a mandibular molar case. Restor Dent Endod. 2020;45(3):e27. https://doi.org/10.5395/rde.2020.45.e27
-
Kim S, Jung H, Kim S, et al. The influence of an isthmus on the outcomes of surgically treated molars: a retrospective study. J Endod. 2016;42(7):1029-1034. https://doi.org/10.1016/j.joen.2016.04.013
-
Lee SM, Yu YH, Wang Y, Kim E, Kim S. The application of "bone window" technique in endodontic microsurgery. J Endod. 2020;46(6):872-880. https://doi.org/10.1016/j.joen.2020.02.009
-
Abella F, de Ribot J, Doria G, et al. Applications of piezoelectric surgery in endodontic surgery: a literature review. J Endod. 2014;40(3):325-332. https://doi.org/10.1016/j.joen.2013.11.014
-
Antal M, Nagy E, Braunitzer G, et al. Accuracy and clinical safety of guided root end resection with a trephine: a case series. Head Face Med. 2019;15(1):30. https://doi.org/10.1186/s13005-019-0214-8
-
Jung RE, Schneider D, Ganeles J, et al. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2009;24(Suppl):92-109.
-
D’Haese J, Van De Velde T, Komiyama A, et al. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clin Implant Dent Relat Res. 2012;14(3):321-335. https://doi.org/10.1111/j.1708-8208.2010.00275.x
-
Vercellotti T, De Paoli S, Nevins M. The piezoelectric bony window osteotomy and sinus membrane elevation: introduction of a new technique for simplification of the sinus augmentation procedure. Int J Periodontics Restorative Dent. 2001;21(6):561-567.
-
Goyal M, Marya K, Jhamb A, et al. Comparative evaluation of surgical outcome after removal of impacted mandibular third molars using a Piezotome or a conventional handpiece: a prospective study. Br J Oral Maxillofac Surg. 2012;50(6):556-561. https://doi.org/10.1016/j.bjoms.2011.10.010
-
Pappalardo S, Guarnieri R. Randomized clinical study comparing piezosurgery and conventional rotatory surgery in mandibular cyst enucleation. J Craniomaxillofac Surg. 2014;42(5):e80-e85. https://doi.org/10.1016/j.jcms.2013.06.013
-
Horton JE, Tarpley TM Jr, Wood LD. The healing of surgical defects in alveolar bone produced with ultrasonic instrumentation, chisel, and rotary bur. Oral Surg Oral Med Oral Pathol. 1975;39(4):536-546. https://doi.org/10.1016/0030-4220(75)90192-9
-
Capuzzi P, Montebugnoli L, Vaccaro MA. Extraction of impacted third molars. A longitudinal prospective study on factors that affect postoperative recovery. Oral Surg Oral Med Oral Pathol. 1994;77():341-343.https://doi.org/10.1016/0030-4220(94)90194-5
-
Ahn SY, Kim NH, Kim S, et al. Computer-aided design/computer-aided manufacturing-guided endodontic surgery: guided osteotomy and apex localization in a mandibular molar with a thick buccal bone plate. J Endod. 2018;44(4):665-670. https://doi.org/10.1016/j.joen.2017.12.009
-
Fernández-Grisales R, Rojas WJ, Berruecos-Orozco C. Piezoelectric endodontic microsurgery with modified cortical window technique: a case report. J Endod Microsurg. 2023;2:34-40. https://doi.org/10.23999/jem.2023.2.4
ABSTRACT IN UKRAINIAN. АНОТАЦІЯ
У цьому звіті про випадок описано нову конструкцію анатомічної направляючої, яка використовується в ендодонтичній мікрохірургії (ЕМ) з технікою кортикального вікна кістки. 60-річна пацієнтка звернувся з постійним болем і рентгенологічним періапікальним ураженням, пов’язаним із зубом 36 (тобто нижнім лівим першим моляром). Після встановлення діагнозу симптоматичного апікального періодонтиту було впроваджено план лікування, що включає керовану ЕМ зі статичною навігацією. Дані конусно-променевої комп’ютерної томографії (КПКТ) були сегментовані для створення стереолітографічного (STL, абревіатура англомовного терміну “stereolithography”) файлу зуба. Цей файл було вирівняно та надруковано на 3D-принтері за допомогою біосумісної смоли, щоб створити індивідуальний анатомічний шаблон. Шаблон полегшив точну остеотомію, точну локалізацію верхівки та консервативне управління клаптем під час операції. Оперативне втручання пройшло успішно, з мінімальними ускладненнями. Контрольна КПКТ через місяць продемонструвала чудову адаптацію кісткового фрагмента та апікального ущільнення. Використання 3D-зображень і індивідуального анатомічного шаблону в ЕМ демонструє багатообіцяючі результати для лікування складних випадків. Запропонована конструкція має переваги, оскільки усуває потребу у направляючих трубках і полегшує консервативне управління клаптем. Рекомендуються подальші клінічні дослідження для підтвердження довгострокової ефективності цієї методики.
ABSTRACT IN SPANISH. RESUMEN
Este informe de caso describe un diseño novedoso para una guía anatómica utilizada en microcirugía endodóncica (ME) con la técnica de ventana de hueso cortical. Una paciente de 60 años presentó dolor persistente y una lesión periapical radiográfica asociada con el diente 36 (es decir, el primer molar inferior izquierdo). Luego de un diagnóstico de periodontitis apical sintomática, se implementó un plan de tratamiento que incluía ME guiada con navegación estática. Los datos de la tomografía computarizada de haz cónico (TCHC) se segmentaron para crear un archivo estereolitográfico (STL, abreviatura del término inglés “stereolitography”) del diente. Este archivo se alineó e imprimió en 3D con una resina biocompatible para crear una guía anatómica personalizada. La guía facilitó una osteotomía precisa, una localización precisa del ápice y un manejo conservador del colgajo durante la cirugía. El procedimiento quirúrgico se completó con éxito, con complicaciones mínimas. La TCHC de seguimiento un mes después demostró una excelente adaptación del fragmento óseo y el sellado apical. El uso de imágenes en 3D y una guía anatómica personalizada en ME demuestra resultados prometedores para el tratamiento de casos complejos. El diseño propuesto ofrece ventajas al eliminar la necesidad de tubos guía y facilitar el manejo conservador del colgajo. Se recomiendan estudios clínicos adicionales para validar la eficacia a largo plazo de esta técnica.