November 3, 2024
J Endod Microsurg. 2024;3: 100016.
Under a Creative Commons license
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2024U000231/
HOW TO CITE THIS ARTICLE (AMA Referencing)
Torres Celeita J, Hernández la Rotta J, Chirinos Salazar A, Fandiño Rodríguez J, López Rincón L, Orduz Solorzano M, Parra Galvis D, Jiménez Peña O. Guided periradicular surgery with Er,Cr:YSGG laser osteotomy: A case report. J Endod Microsurg. 2024;3:100016. https://doi.org/10.23999/j.jem.2024.3.2
ABSTRACT
Purpose: The aim of the study is to observe the bone healing process of a guided periradicular surgery, performed in the endodontics postgraduate course of the University of Santo Tomas, in which an osteotomy was performed for a bone window with erbium, chromium: yttrium, scandium, gallium, garnet (Erbium,Chromium:YSGG) laser (can also be written as Er,Cr:YSGG laser), and the healing process was evaluated by cone-beam computed tomography (CBCT) during the first four months after surgery.
Materials and Methods: After completing the clinical history and studying the CBCT scans, a patient was selected with a diagnosis of symptomatic apical periodontitis, periapical lesion less than 5 mm with intact vestibular cortex that required periradicular surgery due to the presence of an adapted fixed prosthesis and the proximity of the mental foramen to the apex of the tooth to be treated. The treatment plan was established, the surgical guide was designed and the osteotomy was performed with Erbium,Chromium:YSGG laser. The size of the periradicular lesion and the bone density of the surgical area were measured at threepoints in time: pre-surgical (T0), post-surgical at 24 hours (T1), and at 4 months (T2).
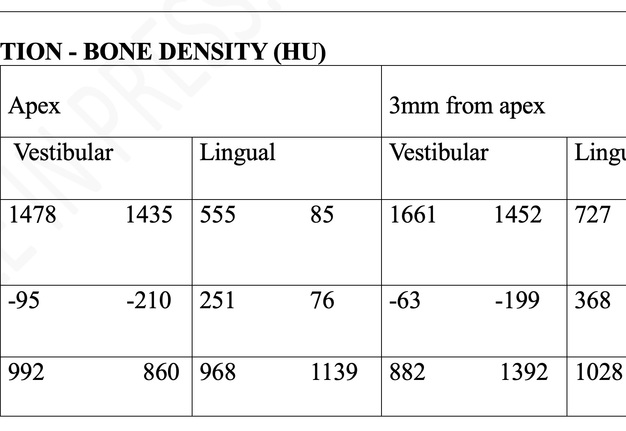
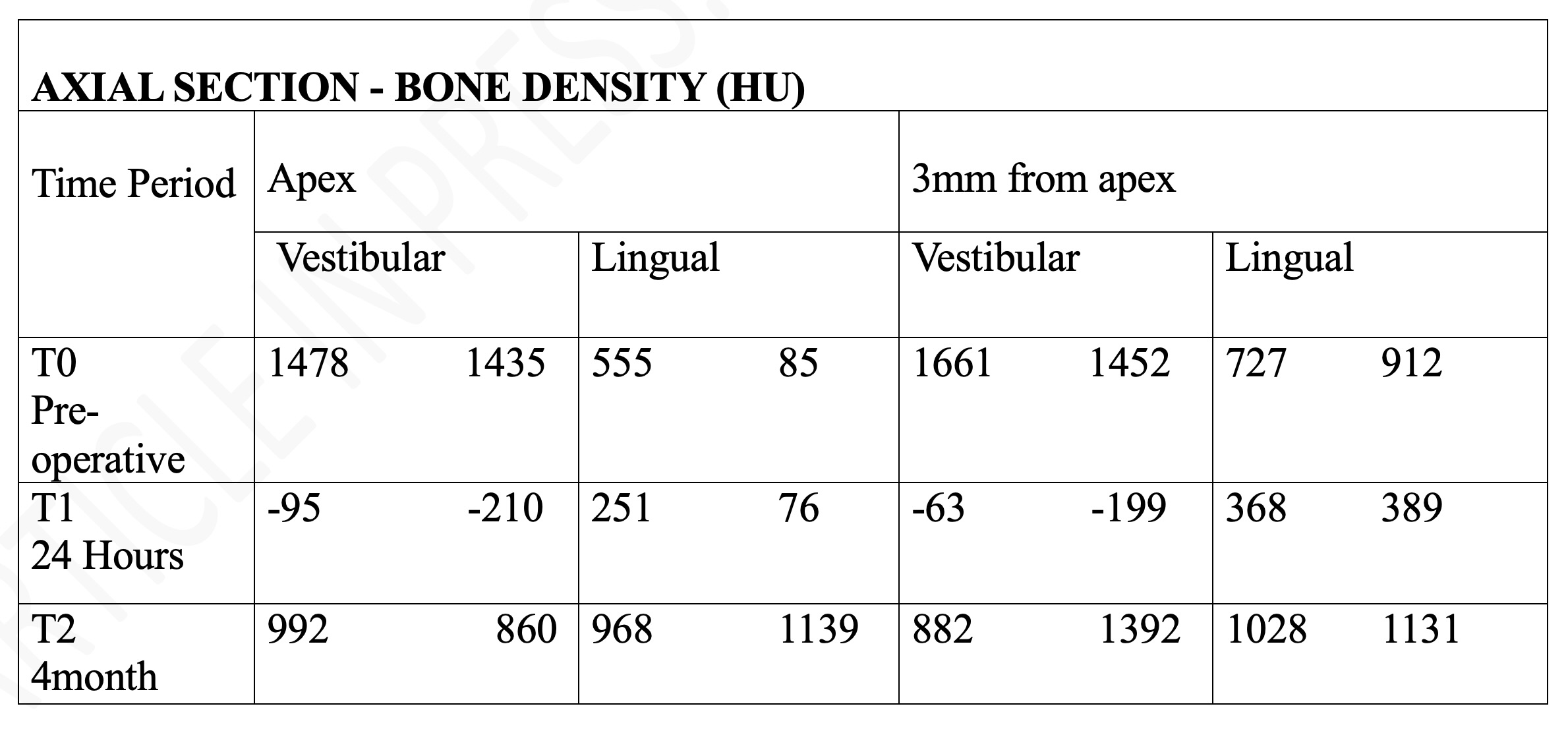
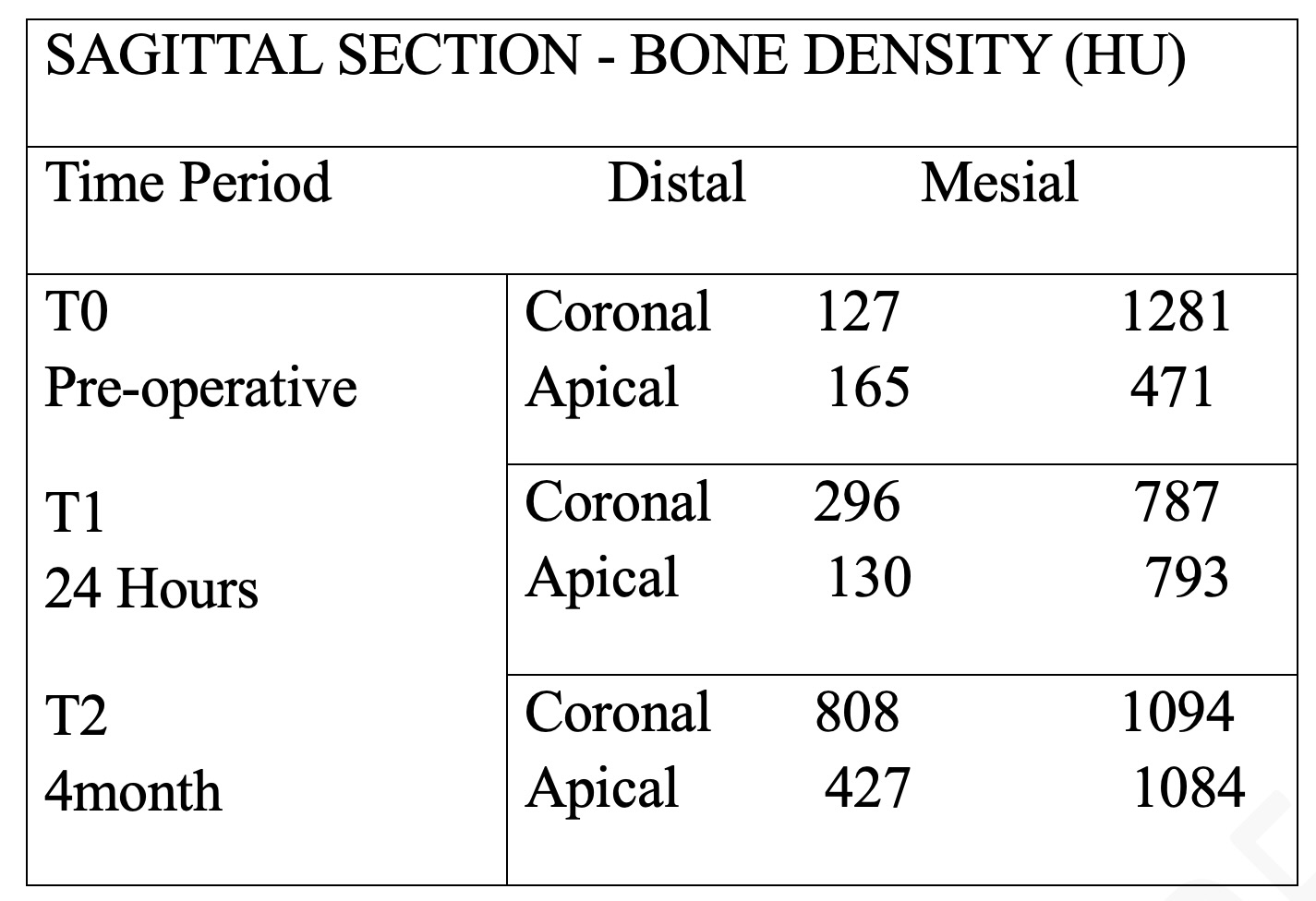
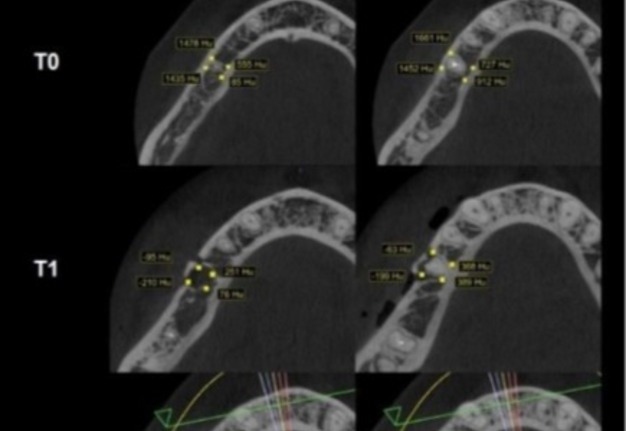
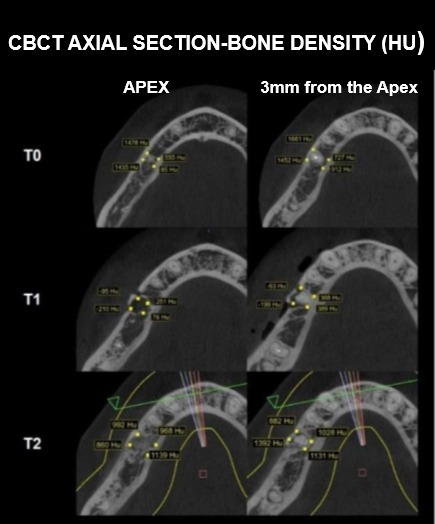
Results: Bone density measured in Hounsfield units (HU) on CBCT in the axial section showed preoperative values in the vestibular apex of 1478 and 1435 HU, at 24 hours after surgery -95 and -210 HU, and in the control at 4 months of 992 and 860 HU. In the coronal slice in the mid vestibular area at the apex level, a preoperative value (T0) of 1335 HU was reported, at 24 hours (T1) -18 HU and at 4 months 1269 HU. At one year of evolution, greater bone density was evidenced comparing between month 4 and month 12.
Conclusions: By performing a surgical procedure with guided technique and Erbium,Chromium:YSGGlaser for the osteotomy, the adverse effects of the surgical procedures are reduced, achieving results with greater accuracy and better prognosis.
KEY WORDS
Er,Cr:YSGG laser, guided periradicular surgery, dental laser, Hounsfield units
INTRODUCTION
Periradicular surgery is one of the options considered to resolve non-surgical endodontic treatment failure and recurrent apical periodontitis when the prognosis of non-surgical retreatment is questionable [1].
We know that the success rate of endodontic microsurgery has increased from 44.2 to 91.1% attributed to technological advances, which allow better visibility during surgery thanks to magnification and direct illumination and the biocompatibility of the materials used [2]. In addition, the use of conventional radiographs provides a two-dimensional view that hinders the precise localization of the lesion; therefore, cone-beam computed tomography (CBCT) is recommended as a complementary tool due to its advantages of showing the exact location of the lesion and its relationship with other anatomical structures, thus allowing precise treatment and post-treatment planning [3-5].
Rubinstein and Kim (2006), suggest that the size of the osteotomy is crucial in the healing process, and advise that the osteotomy should be as small as possible, but wide enough to allow access to the necessary instruments, removal of the periapical lesion and apical resection [5, 6]. It should be noted that the management of freehand periradicular surgery represents greater difficulty when locating the root apex, in addition to the experience of the operator, the technique and the instruments used which are determinant in the amount of alveolar bone removal; This is why guided surgery has been an excellent alternative, which guarantees a more conservative procedure reducing the risk of damage to adjacent anatomical structures, optimizes the time of the procedure, avoids complications and contributes to a better post-surgical prognosis, in addition to improving the healing of the bone defect and reducing postoperative symptoms [7, 8].
Over the years, different techniques have been used to perform osteotomy such as drills, trephine drills, piezoelectric and laser systems [9, 10]. It is also known that the use of rotating parts with drills has been the most used technique; however, it is associated with the generation of heat during the procedure and detritus that increases the inflammatory response with a poor healing process [10-12]. Piezoelectric osteotomy has been used since 2005, with the purpose of minimizing the risks of tissue damage caused by the conventional technique, this is based on ultrasonic microvibrations that through a tip has the ability to cavitate the bone, with the disadvantage of generating too much vibration causing discomfort to the patient [4, 10]. Finally, we have Erbium lasers with wave lengths ranging from 2780 nm to 2940 nm. These lasers have been used in periradicular surgery for approximately two decades [7]. Properly, when used with the proper parameters, a significant decrease in adverse effects has been observed, this is due to the lack of contact with the structures, the reduction of the vibration and reduced heat generation. Thus, as a result, the inflammatory response improves and bacterial filtration after apicoectomy is reduced [13]. Then, its mechanism of action is given by the interaction of Erbium laser with chromophores such as water and hydroxyapatite, through absorption, giving the effect of ablation of mineralized tissues [9, 13]. Thus, thanks to technological advances in bone surgery procedures, a promising alternative to drills, microsaws, trephines and piezosurgery is bone osteotomy by laser [14].
Studies on the use of the Erbium laser in periradicular surgery are limited, which leaves gaps on its different uses and benefits, so studies in this field help to support and give confidence to specialists about the implementation of alternatives in osteotomy during periradicular surgery. Therefore, the objective of this case report is to describe the bone healing process of a guided periradicular surgery with Er,Cr:YSGG laser osteotomy, evaluated by means of CBCT during the first four months after the surgical intervention. The abbreviation Er,Cr:YSGG stands for erbium, chromium: yttrium, scandium, gallium, garnet.
MATERIALS AND METHODS
A descriptive, case report study was performed, approved by the Ethics Committee of the University of Santo Tomas (ethical concept 01952023-3129032032 recorded in minute No. 31 of March 29, 2023, in Bucaramanga). The patients who attended the Endodontics Postgraduate Clinic of the University of Santo Tomas, Bogotá extension, during the year 2023 were then evaluated. The clinical history and digital periapical radiography were duly completed. In addition, CBCT scans were requested, and one patient was selected who met the inclusion criteria: Patient between 25 and 50 years of age, ASA 1 and 2 (according to the American Society of Anesthesiologists [ASA] Classification), diagnosis of asymptomatic or symptomatic apical periodontitis, pulp calcification, with periapical lesion less than 5 mm, intact vestibular cortex and requirement of periradicular surgery. Finally, patients whose teeth had periodontal disease, maladapted restoration, perforation, interradicular retainer with extension to the apical third, fracture of the apical root third or indication for endodontic retreatment were excluded.
CASE REPORT
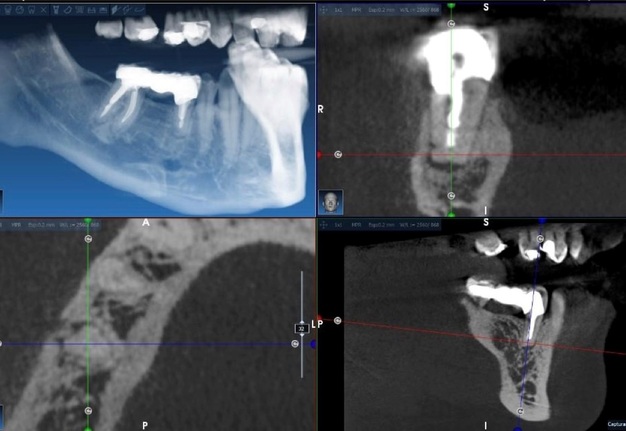
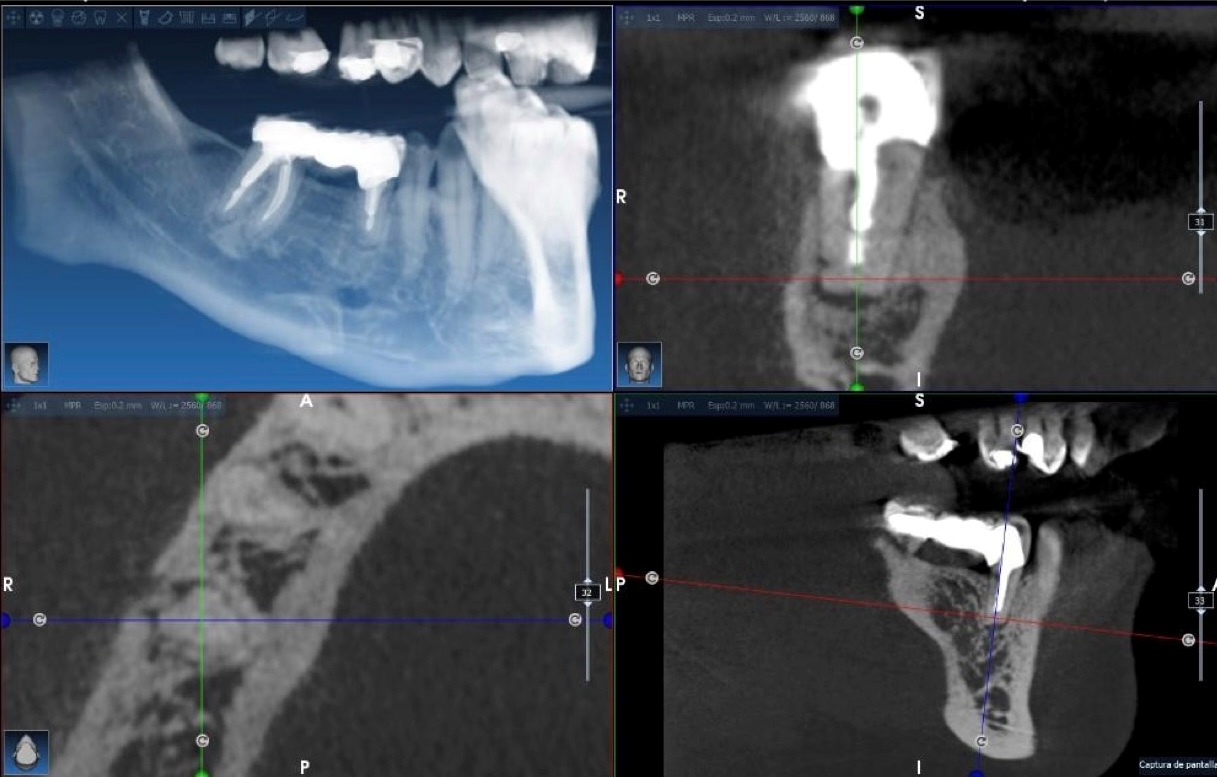
The 30-year-old female patient, who came to the clinic of the Dental Federation for consultation with a history of endodontic and prosthetic treatment performed 4 years ago. The patient reported persistent pain during chewing. Clinical examination revealed a fixed prosthesis from tooth #29 (i.e., tooth #45 according to FDI World Dental Federation notation) to tooth #31 (i.e., tooth #47), with pontic #30 adapted. Tooth #29 (i.e., lower right second premolar) presented mild to moderate pain on percussion, without gingival bleeding or periodontal pockets. There were no signs of inflammation or fistulous tract. Radiographically, tooth #29 showed a radiopaque coronal area consistent with an adapted coronal restoration, a radiopaque area within the canal consistent with an intraradicular post and endodontic filling material, a radiolucent area compatible with an enlarged periodontal ligament space, and the mental foramen in relation to the apex of tooth #29 (Figs 1 and 2).
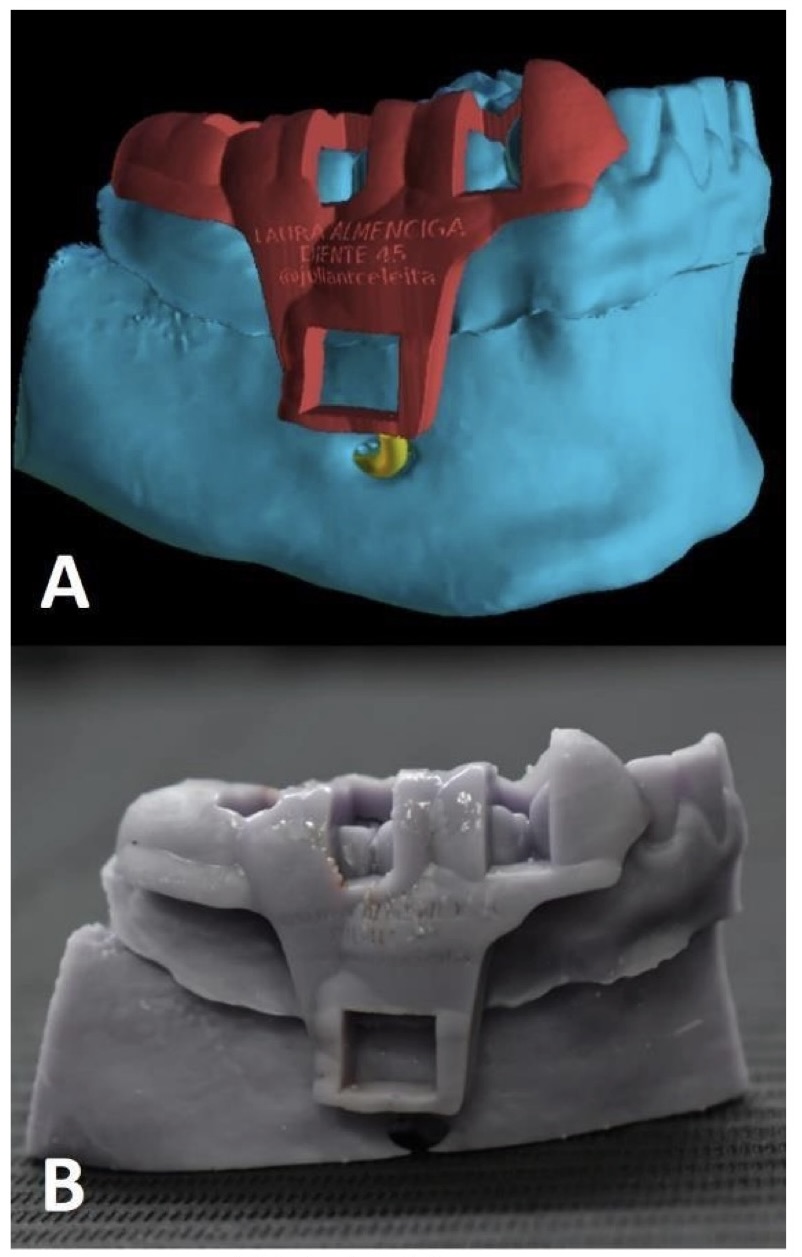
It was decided to perform guided periradicular surgery due to the proximity of the mental foramen to the apex of the tooth #29 (Figs 3 and 4). The patient was informed about the objective of the surgery, the surgical protocol, recovery period, possible complications, accepted and signed the informed consent form containing all the details of the study. Subsequently, an intraoral scan was performed to create the surgical guide. The Digital Imaging and Communications in Medicine (DICOM) files were processed in Blue Sky Plan software (Blue Sky Bio, LLC, Libertyville, IL, United States). The guide was designed (Fig 5A) taking into account the location of the mental foramen, with a surgical window of 4.95 mm high and 6.74 mm wide and then it was printed using a laser printer, and thus we had the essential tool to perform the surgery (Fig 5B).
The variables to be evaluated in this study were bone density, which was measured on CBCT in Hounsfield units (HU), at 3 different times: (T0) pre-surgery, (T1) post-surgery at 24 hours, and (T2) at 4 months.
Surgical Protocol
The patient performed mouthwash with 0.12% chlorhexidine, disinfected extraorally with antiseptic and the fields were placed.
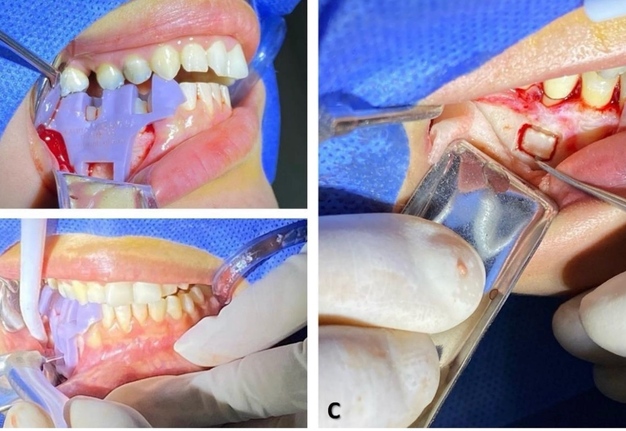
Local anesthesia was administered in the surgical area by means of a truncal block with 4% articaine with 1:100,000 epinephrine and submucosal injections with 2% lidocaine with 1:80,000 epinephrine. The flap design was modified triangular, with intrasulcular access at internal bevel, starting in the distal area of tooth #27 and extending to distal of the pontic of tooth #30. The incision was made with a 15C scalpel blade, and the flap was lifted to full thickness. Finally, the fit of the surgical guide was verified (Fig 6A).
Erbium,Chromium:YSGG Laser Protocol
Laser protective goggles were used on the operator and the patient. The water flow in the Erbium laser (Fig 7) was checked before starting the surgical procedure.
Limited by the window of the surgical guide (6.74mm and 4.95mm), the osteotomy was performed with the 2780 nm Erbium,Chromium:YSGG laser (Waterlase MD; Biolase, Inc., Foothill Ranch,California, United States) with one fiber, MG6 tip, 6 mm length, 3.5 W power, 20 Hz frequency, 55% air, 45% water, H mode, the laser tip is contacted with the bone cortex making firm and continuous movements (Fig 6B,C). The time used to perform the bone window was counted, which was 11'37"73, the bone fragment was removed with the help of a Buser style periosteal elevator and preserved in saline solution.
Periradicular Surgery
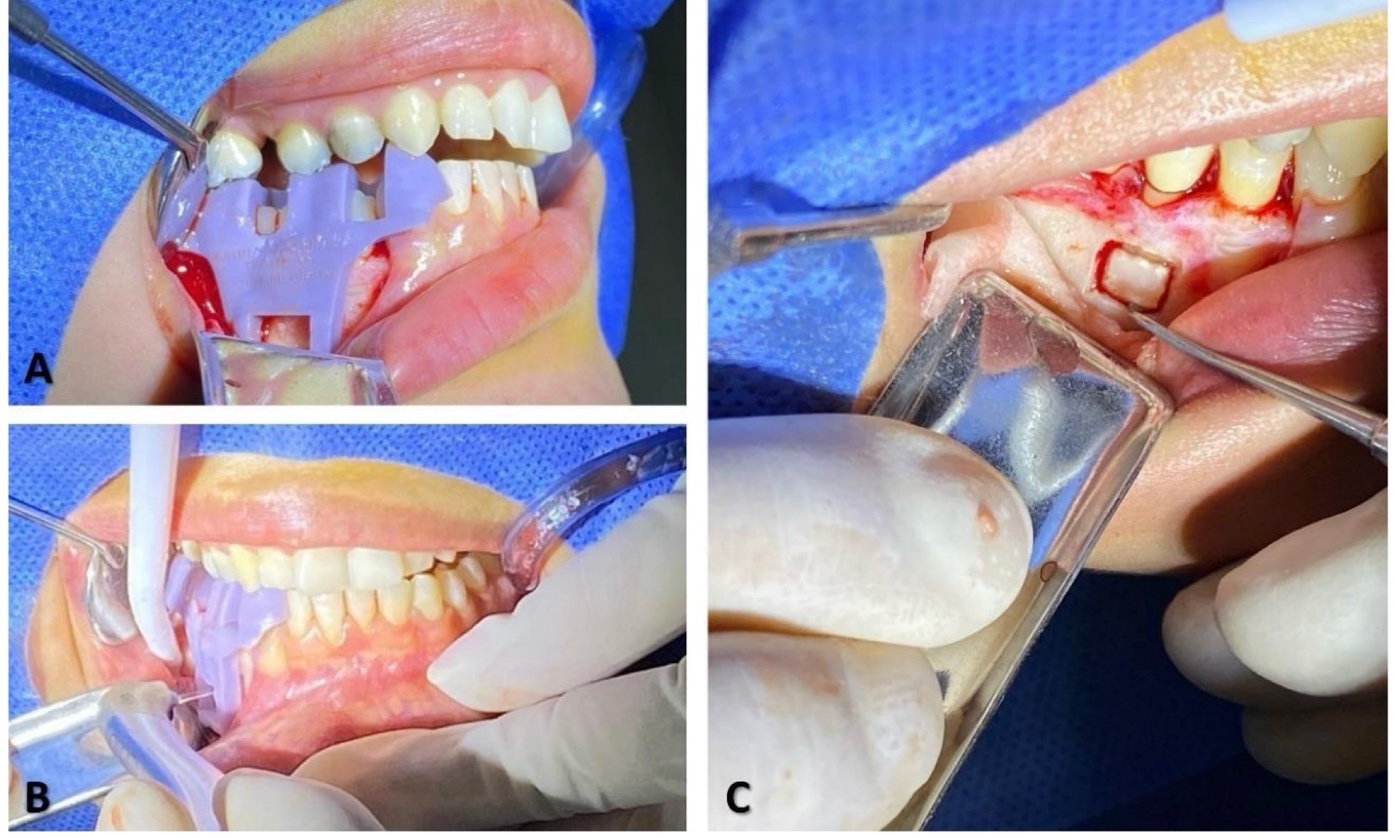
The root apex was checked with methylene blue to rule out possible fractures or fissures and the apical 3 mm were resected by cutting with a Zekrya bur (Fig 8A). The lesion was removed with Lucas curette and hemostasis was performed with sterile gauze impregnated with cold saline. Apical retro-preparation of 3mm was performed with E11D ultrasonic diamond tip and and retro-obturated with Biodentine® bioceramic material (Septodont Ltd., Saint-Maur-des-Fossés, France). Type I collagen sponge was used, the bone cortex was repositioned, the 15 x 20 mm pericardium membrane (bonefill lamina, Bionnovation Biomedical Bauru, São Paulo, Brazil) was positioned, the flap was repositioned and sutured with 6-0 monofilament suture, Polygalactin 910 (Fig 8B-D). Finally, the surgical field was compressed with moist sterile gauze for 3 to 5 minutes for hemostasis.
The following medications were formulated: (1) 500-mg Amoxicillin capsule #21 (1 every 8 hours), (2) 8-mg Dexamethasone ampoule (single dose), and (3) 500-mg Naproxen tablet #9 (1 every 8 hours).
Postoperative Management
CBCT was taken 24 hours after the surgical procedure (T1).
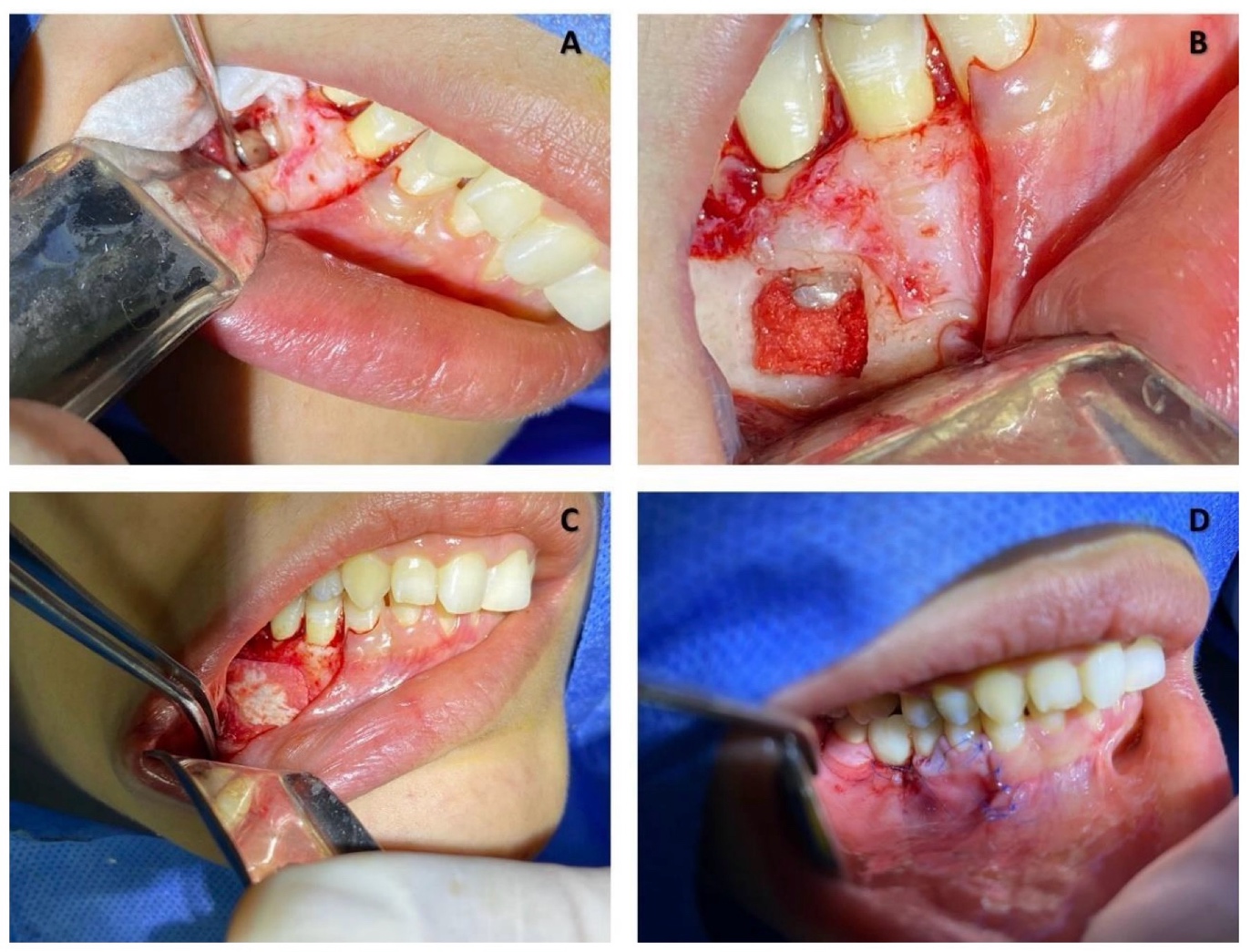
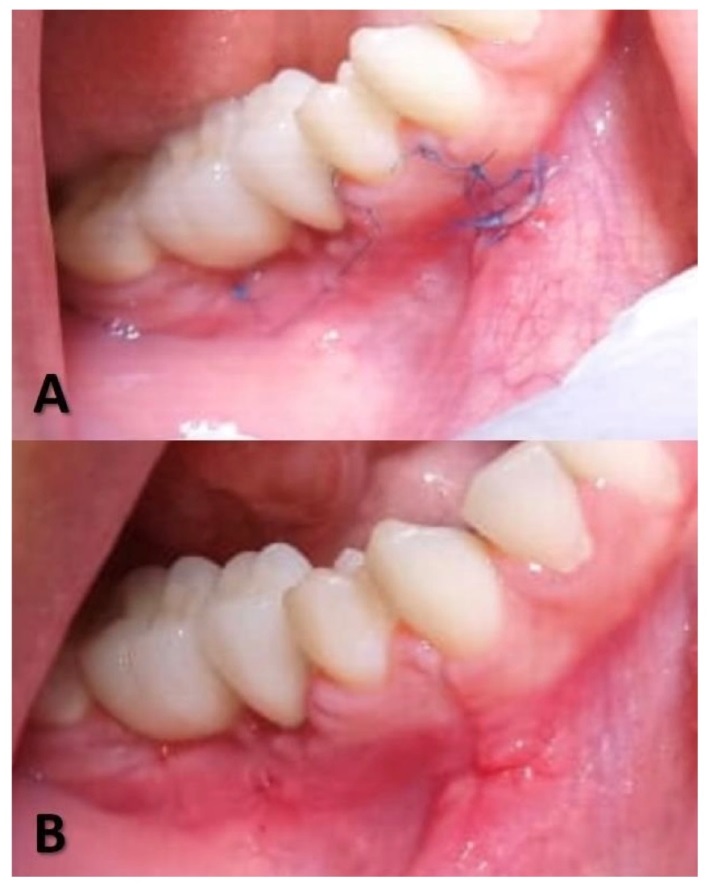
Eight days after surgery, the sutures were removed, and good healing was observed (Fig 9). Figure 10 shows the condition of soft tissues 1 month after the surgery.
At 4 months CBCT (T2) was taken. By means of the Blue Sky Plan software on the CBCT, the bone density of the bone in the surgical area was measured in Hounsfield units (HU).
Bone Density
Bone density values were measured by the same trained operator.
Preoperative and postoperative measurements were taken in different slices (axial, coronal and sagittal) and the results are shown in Tables 1, 2 and 3.
The preoperative bone density in the vestibular axial slice at the apex (T0) was between 1435 and 1478 HU and at 4 months (T2) between 860 and 992 HU. While the initial bone density at 3 mm from the apex in vestibular (T0) was between 1452 and 1661 HU, and at 4 months (T2) was between 882 and 1392 HU. The lowest bone density values in vestibular are reported 24 hours after surgery with negative values between -210 and -95 HU at the apex and at 3 mm from the apex between -199 and -63 HU (Fig 11).
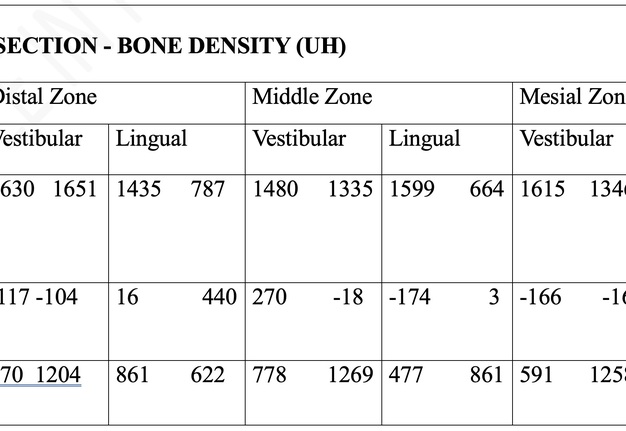
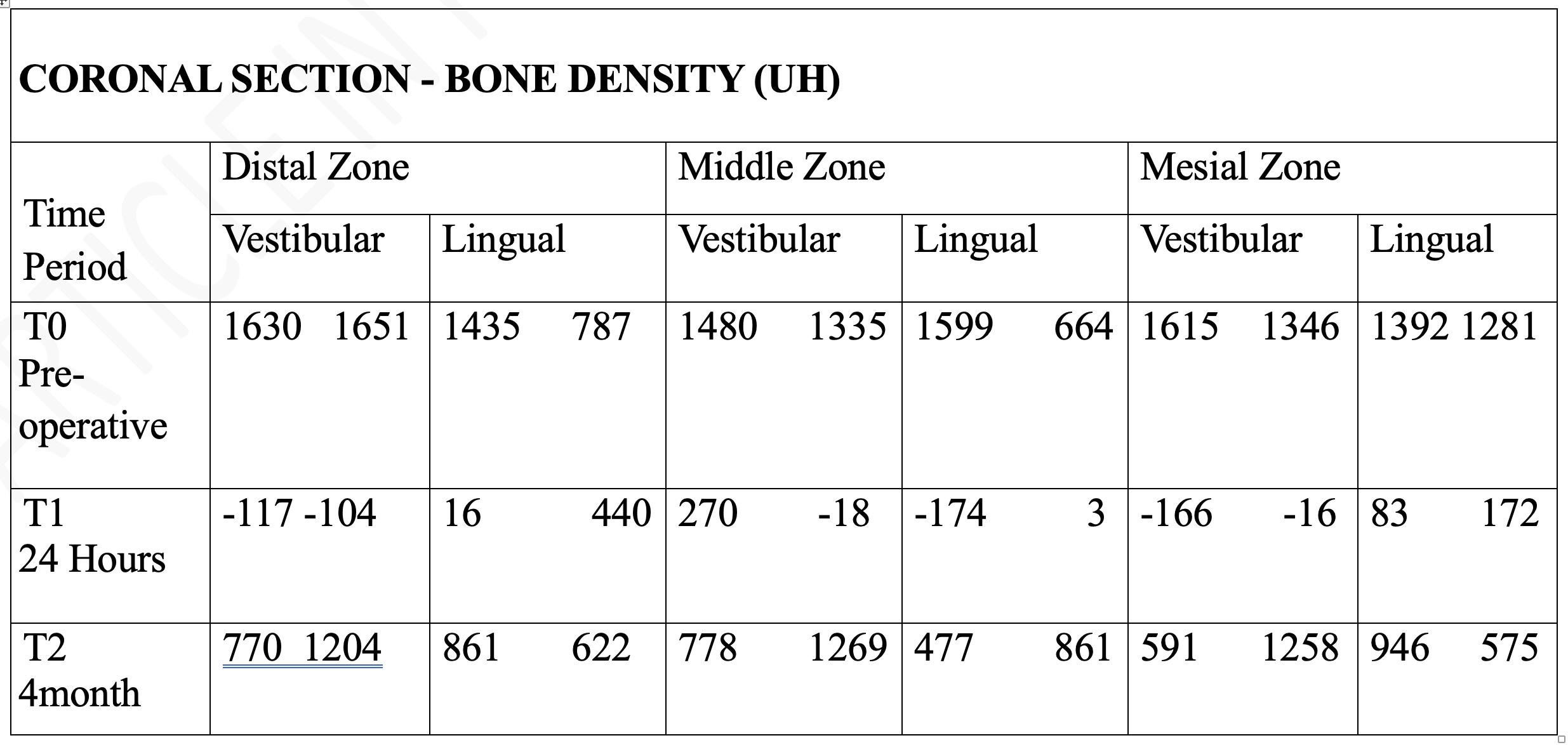
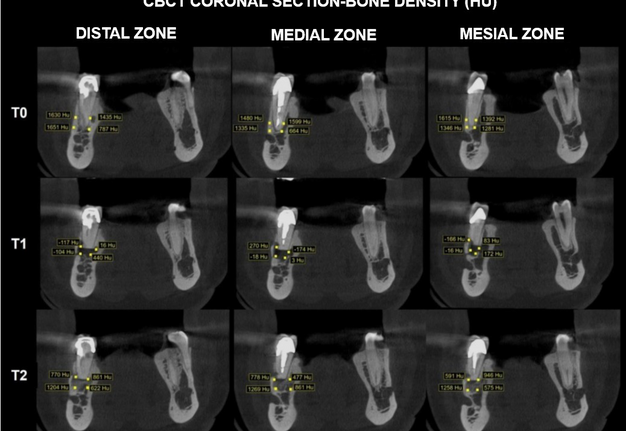
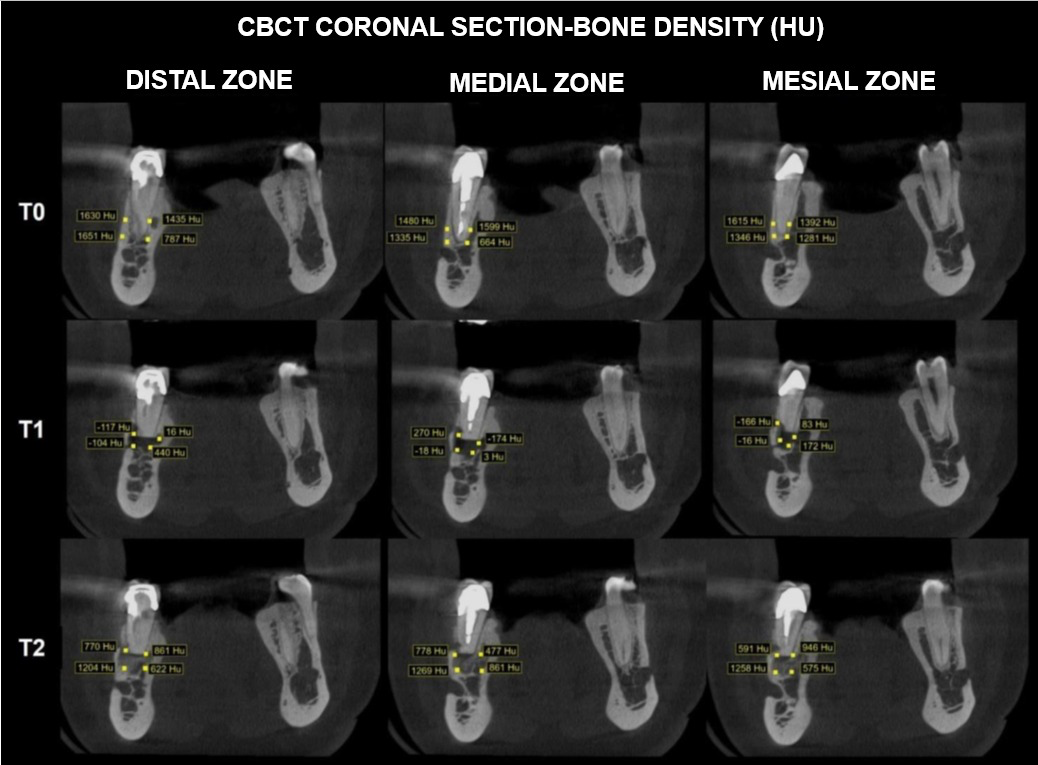
In the different areas (distal, medial and mesial) of the coronal section the preoperative bone density (T0) in vestibular was between 1335 and 1651 HU, at 24 hours after surgery (T1) the values in vestibular were between -166 and 270 HU and in the control at 4 months between 591 and 1269 HU (Fig 12).
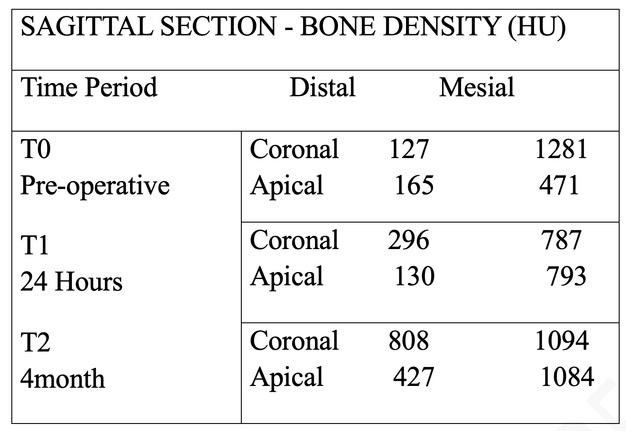
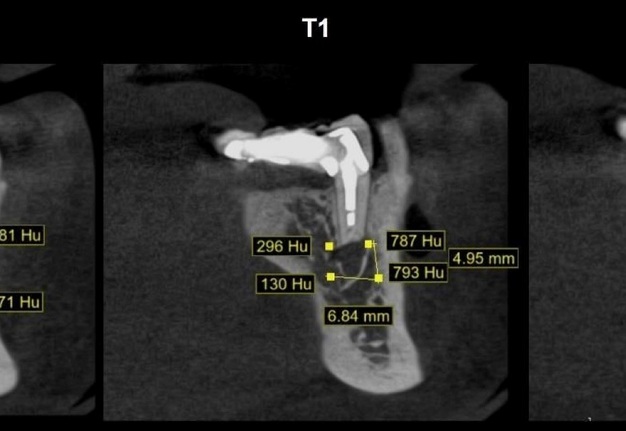
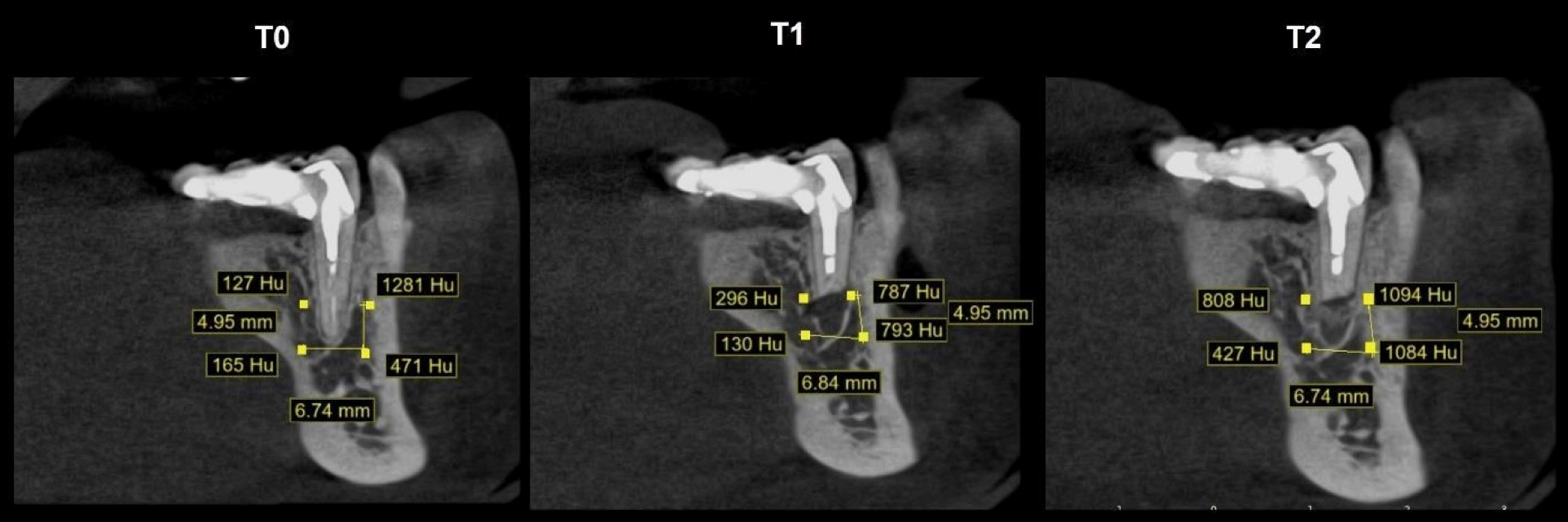
In the sagittal section before surgery (T0) the HU values were between 165 and 1281 HU (average 511 HU), later (T1) between 130 and 793 HU (average 501 HU), and at 4 months (T2) between 427 and 1094 HU (average 853 HU) (Fig 13).
The patient did not report transient paresthesia at any time postoperatively and the follow-up CBCT at 4 months shows satisfactory periapical bone healing, considering that this is the short-term control available.
12-Month Follow-Up
At one year of evolution, greater bone density was evidenced comparing between month 4 and month 12 (Fig 14).
DISCUSSION
Endodontic surgery is defined as the treatment performed on the root apices of an infected tooth that was not resolved with conventional endodontics. In lower posterior teeth this surgery can be more difficult due to limited access, the thickness of the vestibular bone cortex, root morphology and the proximity of the apex to the dental canal and mental foramen [2].
Although there are morphological generalities, each patient presents anatomical variations that may increase the risks during periradicular surgery, therefore, the professional should identify them during the preoperative phase to plan the patient's treatment.
The mental foramen is an important anatomical structure to be taken into account during surgery, being necessary to consider its shape, location, extension of the anterior loop and presence of accessory mental foramina before any surgery to avoid injuring the nerve.
According to a study by Shalash et al. (2020) in a sample of 120 patients, the anterior loop was present in 55% of the cases, while studies report an incidence of accessory mental foramen between 3% and 10.67% which, although smaller, is usually located near the root apex of the second premolars [15]. Therefore, protection of these anatomical structures is important to avoid nerve injury during apical surgery [16].
Regarding the mental foramen in a study by Wang et al. (2017) the results indicated that the majority of the lower posterior teeth can be safely treated by endodontic microsurgery, because the mean distance for most roots with the mental foramen was greater than 5.9 mm, however, that horizontal distance was less than 2 mm in 19.9% of second premolars [16]; Although the debate persists, different studies concluded that in most patients the mental foramen is closer to the second premolar apex [16-20].
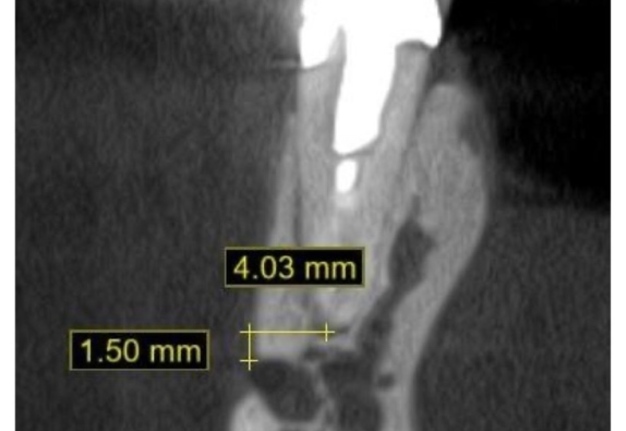
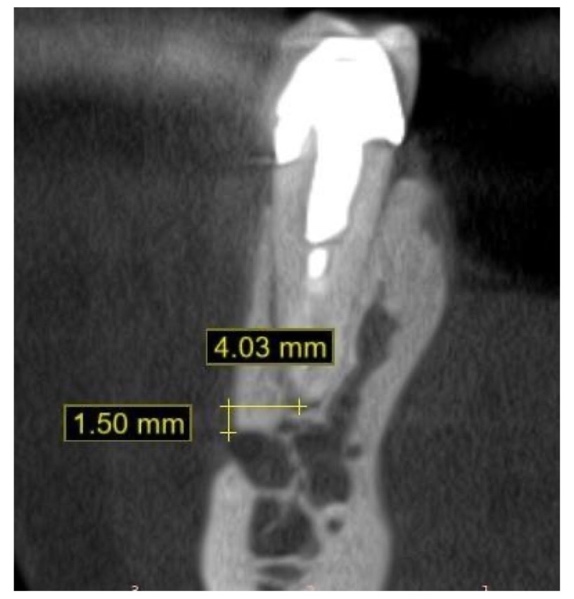
The clinical aspect of this study was the proximity of the mental foramen to the root apex of the tooth to be treated, since the distance measured in the tomography was 1.5 mm (Fig 3); therefore, identifying its exact position with respect to the root apex was important for surgical planning and thus reducing or avoiding damage to the neurovascular bundle that could leave temporary or permanent sequelae in the patient.
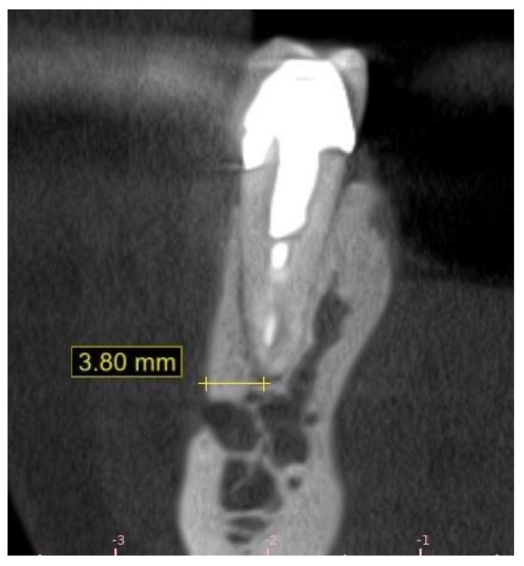
Phillips et al. (1992) in their study on mandibles observed that the radiographic position of the mental foramen was located 3.8 mm mesial to its real location of the tooth apex in 71% of the periapical radiographs examined [21], therefore, measurements on periapical radiographs are not reliable for a surgical approach. In the present clinical case, the use of CBCT was decided for greater planning accuracy.
Pinsky et al. (2007) showed an error of more than 3 mm in 22% of the osteotomies performed freehand and no error with the use of surgical guidance, thus the use of CBCT, surgical guidance together with periradicular microsurgery, are the choice in highly complex cases, and for this reason they were used in the planning and execution of the surgery in the case report of this study [22].
Osteotomy is a surgical procedure in which the bony cortex is removed to establish access to the root apices [16]. Rubinstein and Kim (2002), advise that the osteotomy should be minimal in size, but at the same time and enough extensive to allow adequate visualization and access to the instruments required to treat the tissues [6, 10]. Among the disadvantages of performing freehand osteotomy is damage to anatomically important structures and increased size of the bony defect, which is associated with unsuccessful, uncertain or delayed healing, and increased risk of postoperative complications [23, 24]. In this study, trauma was minimized by using surgical guidance to perform the bony window over the apex, taking into account that the vestibular cortical bony plate was intact. The osseous window measured 6.74 mm and 4.95 mm.
In addition, it was taken into account at the time of the osteotomy that fractures can occur due to the contact pressure exerted by the cutting instrument and the vibration generated by mechanical instruments [8], being important to highlight that the friction generated with the conventional method can cause pain, thermal damage to the surrounding tissue, chip deposition and bacterial contamination [25]. Some authors have demonstrated positive effects on bone healing derived from the use of piezoelectric compared to conventional mechanical methods [25-27]. However, studies such as that of Pandurić et al. (2012) performed on pig ribs and that of Pandarathodiyil et al. (2020) highlight that Erbium laser osteotomy, has no direct contact with the structures, offers a regular cut, operative field free of impurities, absence of carbonization, short time for its execution and elimination of the smear layer that allow the blood cells to adhere more easily on the intervened surface resulting in a better healing process [28, 29]. Studies in animal models have shown that the irradiation generated with the Er,Cr:YSGG laser stimulates the secretion of platelet-derived growth factor, reinforcing the premise of improved healing at the intervened site [30]. Thanks to the incorporation of high energy lasers for bone surgery procedures in the last decades, it is possible to highlight the properties of the Erbium laser in these treatments. Also, studies speak of the advantages of using the Erbium laser in periradicular surgery compared to conventional surgical procedures, such as the tendency to less bleeding, less tissue trauma of surrounding tissues, absence of vibrations and less heat production in hard tissues [13]; mentioned benefits, it was chosen to perform the osteotomy of the periradicular surgery of this case report with the Er,Cr:YSGG laser, being evident during the procedure the low presence of bleeding, uniform cutting of the bone tissue and the minimum generation of bone spicules or fragments, its easy handling, absence of necrosis and carbonization zone due to the constant irrigation of the Erbium laser that avoids overheating of the bone.
The use of the Erbium laser has been reported since 1960 and has been investigated and used in a wide variety of wavelengths depending on the requirement, whether for coagulation, vaporization and ablation of hard and soft tissues [26]. The Er,Cr:YSGG is of infrared energy distribution with a wavelength of 2780 nm, non-ionizing, pulsed emission, and its active medium consists of Erbium (Er), Chromium (Cr), Yttrium (Y), Scandium (S), the Gallium (G), and Garnet (G), and is provided with an aerosol of water and air, which in combination with the light beam, cools the area of incidence, which minimizes the thermal effects and enhances its mechanism of action, for a variety of intraoral applications [31, 32].
On the other hand, the interaction between the Erbium laser and chromophores present in the tissue, such as water and hydroxyapatite, occurs through a thermomechanical ablation mechanism. This phenomenon is commonly known as “water molecule explosion”, where surface water in the tissue matrix undergoes a rapid increase in temperature, resulting in increased molecular vibration and consequently an increase in surface pressure [33].
In a study carried out in rabbits by De Santis et al. (2018) selected five instruments for osteotomy used in dentistry (burr, Piezosurgery I, Piezosurgery II, erbium-doped yttrium aluminium garnet laser [Er:YAG laser], and Er,Cr:YSGG laser) with which they evaluated the cutting characteristics in vivo and in vitro; the results showed that the width of the cut represents an increased risk of rupture depending on the caliber and vibrations of the instrument during osteotomy, the burr obtained the highest values, followed by Piezosurgery I, Piezosurgery II, and Er:YAG laser, and the lowest risk was evidenced with the use of the Er,Cr:YSGG laser [34]. The number of repetitions was also evaluated giving as results higher number of interventions recorded in both piezoelectric devices to perform the same osteotomy. Finally, the data regarding osteotomy time showed some significant differences between the devices.
The drill needs twice less time than Piezosurgery I and Er,Cr:YSGG laser and three times less time than Piezosurgery II and Er:YAG laser to execute the same procedure [34]. The Er,Cr;YSGG laser osteotomy performed in this case report took 11 minutes and 37 seconds, which is considered an optimal time for this procedure if one seeks to generate the least tissue damage. However, this time is influenced by several factors, including the size of the bony window, the thickness of the osseous cortex, the complexity of accessing the site to be intervened, and the additional caution due to the proximity of the mental foramen.
De Santis et al. also analyzed the surface morphology of the cut and examined them with optical microscopy, and observed that the drill is less precise, generates irregular edges and tears the periosteal tissue, while the piezoelectric I and II allow straighter cuts, and both lasers generate slightly wavy cut edges, due to the absence of direct contact of the device and the physiological fluctuations of the operator's hand [34]. Thus, they conclude that the drill produces a large amount of small debris that obstructs the medullary spaces, the Piezosurgery II generates abundant detritus due to the type of vibration, and, on the contrary, this eventuality is almost completely absent with the laser and Piezosurgery I, these devices generate a lower amount of detritus, substantially preserving the medullary spaces [34]. The study points out that, although the piezoelectric and Erbium laser demonstrate advantages, their high acquisition cost and the need for specific training continue to limit their use among professionals, in addition to highlighting that the Erbium laser has advantages in case of risky interventions near to anatomical landmarks [34]. For this study, the Er,Cr;YSGG Laser was chosen, but, the choice of the instrument to perform the osteotomy is going to depend on the experience of the operator and the characteristics of the intervention. For this reason, before the patient was operated on, a pilot test was performed on pig mandibles to perform osteotomies with the Er,Cr:YSGG laser.
In their study, De Oliveira et al. (2016), highlight that one of the limitations of the use of the Er,Cr:YSGG laser for bone tissue ablation are the time required to remove the desired tissue compared to drills mounted on high-speed handpieces [35]; However, the alteration in the pulsed mode of lasers proved to be an alternative to accelerate the ablation of bone tissue and, thus, solve this limitation, furthermore they refer that it is likely that the irregularities observed after Laser irradiation in their study are beneficial for healing because they facilitate the adhesion of the fibrin network, which represents the first event of hard tissue healing [35].
Thus, it should be evaluated whether the time taken to achieve osteotomy really represents.
A disadvantage versus the described benefits of Er,Cr:YSGG laser in performing osteotomy. HU scanning is used to distinguish tissue types, such as cysts from granulomas, e.g., air = -1000 HU, water = 0 HU, muscle = +40 HU, and bone >+400 HU [36]. Some studies suggest that scatter and artifacts have undesirable impacts on the reliability of HU values in CBCT images and this is why HU values are applied over CT. However, there are also several studies reporting that HU values could be used to assess bone density in CBCT images with certain advantages over multi-slice computed tomography (MSCT), such as high resolution, potentially lower radiation doses and reduced costs [37], so it remains the best available method to monitor bone mineral density changes, provided that the same CBCT machine and scanning configuration are used [38]. In the methodology used for this study, the same tomographic equipment was used with the same image acquisition setup, patient head posture and fields of view (FOV) during image acquisition to minimize problems associated with the technique.
The HU depends on the composition and nature of the tissue being imaged, thus denser tissue (higher absorption of the X-ray beam) has positive values, while less dense tissue (lower absorption) has negative values, where distilled water is arbitrarily defined as zero HU and air as -1000 HU. Upper limits can reach up to 1000 HU for bone, 2000 HU for dense bone such as the cochlea, over 3000 HUfor metals and muscle 40 HU [36, 39]. Continuing advances in computed tomography (CT) as a diagnostic tool have resulted in different CT designs. In turn, different CT designs may alter HU. For example, CBCT, used primarily in dentistry, cannot show true HU similarly to conventional CT, but does show a strong correlation [39]. In this case report, in the axial section, preoperative values (T0) in vestibular at the apex of 1478 and 1435 HU were recorded, which after periradicular surgery (T1) were -95 and -210 HU, and in the 4-month control (T2) positive values of 992 and 860 HU were again recorded, Similarly, in the coronal section in the mid vestibular area at the apex level, a preoperative value (T0) of 1335 HU was reported, which 24 hours after periradicular surgery (T1) was -18 HU and at 4 months 1269 HU. The negative values correspond to the space due to the apical resection of the root and the positive values after 4 months show a real healing process in the area of the apical resection.
A study by Goyushov et al. (2023) measured periapical bone density in lower teeth with CBCT. The mean value of HU in the periapices of premolars was 470.58 HU [37]. In the present case report the HU values taken in the sagittal cut before surgery (T0) had an average of 511 HU, at 24 hours (T1) average of 501 HU, and in the control at 4 months (T2) an average of 853 HU, these values were measured taking into account the size of the surgical guide that was used to make the bone window, HU values at the three moments do not show negative values, and the average HU before and 24 hours after surgery is similar indicating that the osteotomy was kept within the limits of the surgical guide preserving the bone tissue and taking care not to lacerate the mental nerve.
The use of HU to measure tissue density has aided radiologists in image interpretation and disease diagnosis, and is used in different specialties of medicine, for example in the diagnosis of fatty liver, predictor of growth in meningiomas, differential diagnosis of odontogenic cysts, determine bone density, estimate bone quality prior to spinal instrumentation, predict pedicle screw loosening and in degenerative lumbar scoliosis, among many other uses [39], such as assessing bone quality prior to implant surgery, particularly immediate implantation, it has been shown that primary implant stability improves with higher peri-implant bone density (higher HU values) [37]. The use of these tools is useful to establish whether new technologies really favor and accelerate the bone healing process.
CONCLUSIONS AND RECOMMENDATIONS
From the clinical case report it is highlighted that the patient did not manifest neural alteration, and the postoperative symptomatology was very positive. Even, in the control performed at 4 months the patient did not present pain on percussion or chewing. The clinical and tomographic healing process up to 4 months has been positive. It is recommended to perform controls at 8 months, 1, 2, and 5 years.
In the same line, it was observed that by performing a surgical procedure with a guided technique and with Erbium laser for the osteotomy, the adverse effects of the surgical procedures are reduced, achieving results with greater accuracy and better prognosis.
On the other hand, guided periradicular surgery is an excellent alternative in cases without fenestration that helps to minimize the extension of the osteotomy, facilitates the location of the pathologic process area and protects nerve structures. Likewise, the Er,Cr:YSGG laser is useful for professionals in oral surgical procedures because it favors better healing by generating fewer adverse effects, due to the fact that it ablates the tissue through absorption by chromophores. Moreover, more studies using the Er,Cr:YSGG laser in osteotomy during periradicular surgery with a larger sample size and comparing it with other techniques are required to determine if the advantages offered by the laser in the healing process are statistically significant.
Finally, to know how to measure bone density as a Hounsfield units can be useful as a diagnostic tool and provide information that allows the modification of surgical techniques.
CONFLICT OF INTEREST
The authors declare that they don’t have any conflicts of interest.
REFERENCES (39)
-
Lee SM, Yu YH, Wang Y, et al. The application of "bone window" technique in endodontic microsurgery. J Endod. 2020;46(6):872-880. https://doi.org/10.1016/j.joen.2020.02.009
-
Oliva LER, Elizondo JE, Rangel SS, et al. An update on guided endodontics. Int J Appl Dent Sci.2023;9(3):98-101. https://doi.org/10.22271/oral.2023.v9.i3b.1792
-
Connert T, Krug R, Eggmann F, et al. Guided endodontics versus conventional access cavity preparation: A comparative study on substance loss using 3-dimensional-printed teeth. J Endod. 2019;45(3):327-331. https://doi.org/10.1016/j.joen.2018.11.006
-
Rashad A, Sadr-Eshkevari P, Heiland M, et al. Practitioner experience with sonic osteotomy compared to bur and ultrasonic saw: a pilot in vitro study. Int J Oral Maxillofac Surg. 2015;44(2):203-208. https://doi.org/10.1016/j.ijom.2014.09.004
-
Rashmi S, Saini KrV. Guided osteotomy: A conservative method for periapical surgery with the aid of cone-beam computed tomography and three-dimensional printing technology. Tanta Dent J. 2022;19(3):172-176. https://doi.org/10.4103/tdj.tdj_8_22
-
Rubinstein RA, Kim S. Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod. 2002;28(5):378-383. https://doi.org/10.1097/00004770-200205000-00008
-
Angiero F, Benedicenti S, Signore A, et al. Apicoectomies with the erbium laser: a complementary technique for retrograde endodontic treatment. Photomed Laser Surg. 2011;29(12):845-849. https://doi.org/10.1089/pho.2011.3046
-
Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod. 2006;32(7):601-623. https://doi.org/10.1016/j.joen.2005.12.010
-
Martins GL, Puricelli E, Baraldi CE, Ponzoni D. Bone healing after bur and Er:YAG laser ostectomies. J Oral Maxillofac Surg. 2011;69(4):1214-1220. https://doi.org/10.1016/j.joms.2010.02.029
-
Vargas-Buratovic JP, López-Suárez CP, Rojas-Bascuñán AS, Pinedo-Henríquez FJ. Piezoelectric bone surgery compared to conventional saw in orthognathic surgery. Int J Interdiscip Dent. 2021;14(1):73-78. In Spanish. https://doi.org/10.4067/S2452-55882021000100073
-
Stübinger S. Advances in bone surgery: the Er:YAG laser in oral surgery and implant dentistry. Clin Cosmet Investig Dent. 2010;2:47-62. https://doi.org/10.2147/CCIDE.S8352
-
Tsesis I, Rosen E, Taschieri S, et al. Outcomes of surgical endodontic treatment performed by a modern technique: an updated meta-analysis of the literature. J Endod. 2013;39(3):332-339. https://doi.org/10.1016/j.joen.2012.11.044
-
Komori T, Yokoyama K, Takato T, Matsumoto K. Clinical application of the erbium:YAG laser for apicoectomy. J Endod. 1997;23(12):748-750. https://doi.org/10.1016/s0099-2399(97)80348-2
-
Romanos GE. Advanced laser surgery in dentistry. Hoboken, NJ: Wiley-Blackwell; 2021.
-
Shalash M, Khallaf ME, Ali AR. Position and dimensions of the mental foramen and presence of the anterior loop in the Egyptian population: a retrospective CBCT study. Bull Natl Res Cent. 2020: 44, 110. https://doi.org/10.1186/s42269-020-00364-2
-
Wang X, Chen K, Wang S, et al. Relationship between the mental foramen, mandibular canal, and the surgical access line of the mandibular posterior teeth: A cone-beam computed tomographic analysis. J Endod. 2017;43(8):1262-1266. https://doi.org/10.1016/j.joen.2017.03.043
-
Bürklein S, Grund C, Schäfer E. Relationship between root apices and the mandibular canal: A cone-beam computed tomographic analysis in a German population. J Endod. 2015;41(10):1696-1700. https://doi.org/10.1016/j.joen.2015.06.016
-
Chong BS, Gohil K, Pawar R, Makdissi J. Anatomical relationship between mental foramen, mandibular teeth and risk of nerve injury with endodontic treatment. Clin Oral Investig. 2017;21(1):381-387. https://doi.org/10.1007/s00784-016-1801-8
-
Ngeow WC, Yuzawati Y. The location of the mental foramen in a selected Malay population. J Oral Sci. 2003;45(3):171-175. https://doi.org/10.2334/josnusd.45.171
-
Pelé A, Berry PA, Evanno C, Jordana F. Evaluation of mental foramen with cone beam computed tomography: A systematic review of literature. Radiol Res Pract. 2021;2021:8897275. https://doi.org/10.1155/2021/8897275
-
Phillips JL, Weller RN, Kulild JC. The mental foramen: Part II. Radiographic position in relation to the mandibular second premolar. J Endod. 1992;18(6):271-274. https://doi.org/10.1016/s0099-2399(06)80953-2
-
Pinsky HM, Champleboux G, Sarment DP. Periapical surgery using CAD/CAM guidance: preclinical results. J Endod. 2007;33(2):148-151. https://doi.org/10.1016/j.joen.2006.10.005
-
Fernández-Grisales R, Rojas WJ, Berruecos-Orozco C. Piezoelectric endodontic microsurgery with modified cortical window technique: a case report. J Endod Microsurg. 2023;2:34-40. https://doi.org/10.23999/jem.2023.2.4
-
Kim U, Kim S, Kim E. The application of "bone window technique" using piezoelectric saws and a CAD/CAM-guided surgical stent in endodontic microsurgery on a mandibular molar case. Restor Dent Endod. 2020;45(3):e27. https://doi.org/10.5395/rde.2020.45.e27
-
Cervera Ballester J, Menéndez Nieto I, Soto Peñaloza D, et al. New perspectives in periapical surgery: Ostectomy and osteotomy. J Oral Science Rehabilitation. 2019;5(1): 8-17.
-
Stübinger S, Nuss K, Pongratz M, et al. Comparison of Er:YAG laser and piezoelectric osteotomy: An animal study in sheep. Lasers Surg Med. 2010;42(8):743-751. https://doi.org/10.1002/lsm.20946
-
Tortorici S, Difalco P, Caradonna L, Tetè S. Traditional endodontic surgery versus modern technique: A 5-year controlled clinical trial. J Craniofac Surg. 2014;25(3):804-807. https://doi.org/10.1097/scs.0000000000000398
-
Pandarathodiyil AK, Anil S. Lasers and their applications in the dental practice. Int J Dentistry Oral Sci. 2020;7(11):936-943.
-
Pandurić DG, Bago I, Katanec D, et al. Comparison of Er:YAG laser and surgical drill for osteotomy in oral surgery: An experimental study. J Oral Maxillofac Surg. 2012;70(11):2515-2521. https://doi.org/10.1016/j.joms.2012.06.192
-
Kesler G, Shvero DK, Tov YS, Romanos G. Platelet derived growth factor secretion and bone healing after Er:YAG laser bone irradiation. J Oral Implantol. 2011;37 Spec No:195-204. https://doi.org/10.1563/AAID-JOI-D-09-00120.1
-
Fekrazad R, Moharrami M, Chiniforush N. The esthetic crown lengthening by Er;Cr:YSGG laser: A case series. J Lasers Med Sci. 2018;9(4):283-287. https://doi.org/10.15171/jlms.2018.50
-
Kumar G, Rehman F, Chaturvedy V. Soft tissue applications of Er,Cr:YSGG laser in pediatric dentistry. Int J Clin Pediatr Dent. 2017;10(2):188-192. https://doi.org/10.5005/jp-journals-10005-1432
-
Schwarz F, Arweiler N, Georg T, Reich E. Desensitizing effects of an Er:YAG laser on hypersensitive dentine. J Clin Periodontol. 2002;29(3):211-215. https://doi.org/10.1034/j.1600-051x.2002.290305.x
-
De Santis D, Gerosa R, Zanotti G, et al. Experimental analysis about the evaluation of tungsten carbide-bur, piezoelectric and laser osteotomies. Minerva Stomatol. 2013;62(8 Suppl 1):9-17.
-
de Oliveira GJ, Rodrigues CN, Perussi LR, et al. Effects on bone tissue after osteotomy with different high-energy lasers: An ex vivo study. Photomed Laser Surg. 2016;34(7):291-296. https://doi.org/10.1089/pho.2015.3917
-
Kaya S, Yavuz I, Uysal I, Akkuş Z. Measuring bone density in healing periapical lesions by using cone beam computed tomography: A clinical investigation. J Endod. 2012;38(1):28-31. https://doi.org/10.1016/j.joen.2011.09.032
-
Goyushov S, Asar NV, Tözüm TF. Assessment of radiodensity at mandibular periapical bone sites using three-dimensional cone-beam computed tomography. J Oral Maxillofac Res. 2023;14(1):e2. https://doi.org/10.5037/jomr.2023.14102
-
Vitral RW, Fraga MR, da Silva Campos MJ. Use of Hounsfield units in cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2015;148(2):204. https://doi.org/10.1016/j.ajodo.2015.05.005
-
DenOtter TD, Schubert J. Hounsfield unit. In: StatPearls. Treasure Island (FL): StatPearls Publishing; March 6, 2023.