Endodontic Microsurgery of a Mandibular Molar Using a Dynamic Navigation System (DNS) and Cortical Window Technique: A Case Report
August 2, 2024
J Endod Microsurg. 2024; 3: 100018.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE (AMA Referencing)
Castillo GA, Restrepo-Méndez SA, Zuluaga OE, Escobar-Villegas PA. Endodontic microsurgery of a mandibular molar using a dynamic navigation system (DNS) and cortical window technique: A case report. J Endod Microsurg. 2024;3:100018. https://doi.org/10.23999/j.jem.2024.3.5
NATIONAL REPOSITORY OF ACADEMIC TEXTS
https://nrat.ukrintei.ua/en/searchdoc/2024U000230/
ABSTRACT. ABSTRACT IN UKRAINIAN (PDF). ABSTRACT IN SPANISH (PDF).
Recent advancements in endodontic surgery have significantly improved outcomes through enhanced technology, including digital planning, cone-beam computed tomography (CBCT), and operating microscopes. The integration of dynamic navigation systems (DNS) has particularly transformed endodontic microsurgery (EM) by providing real-time guidance and precision. This case report explores the application of DNS in a clinical case of EM involving a mandibular first molar with symptomatic apical periodontitis. A 36-year-old male patient presented with masticatory pain in the lower left quadrant. Radiographic and CBCT evaluations revealed an underfilled mesiolingual canal and a periapical lesion. The surgical procedure utilized DNS for precise osteotomy and apicectomy, guided by the Navident® system and incorporating the cortical window technique. Postoperative care included antibiotic therapy and follow-up appointments, demonstrating successful periapical healing at 21 months. DNS technology significantly enhances precision and conservativeness in EM, allowing for real-time guidance and minimizing iatrogenic risks. The cortical window technique, combined with DNS, facilitates effective root access while preserving bone structure. Despite its advantages, DNS is associated with high costs and a steep learning curve. Future research should focus on evaluating the long-term clinical outcomes of DNS, improving system usability, and exploring its applications in other endodontic procedures. This case report demonstrates the successful use of DNS in conjunction with the cortical window technique for EM, achieving favorable clinical outcomes and promoting accelerated healing. Further studies are needed to validate the broader clinical utility of DNS and to refine its integration into routine practice.
Keywords
Apicoectomy, surgery, computer-assisted, case reports, microsurgery, osteotomy, cone-beam computed tomography
INTRODUCTION
The endodontic surgery field has evolved due to technological advancements in various equipment, diagnostic aids, techniques, and materials. More recently, the implementation of digital planning has favored the execution, predictability, and prognosis of the procedure [1]. The transition to computer aided 3D systems have represented a breakthrough, leading to higher success rates compared to conventional endodontic surgery [2].
Cone-beam computed tomography (CBCT) and magnification have become indispensable tools in endodontic microsurgery (EM). The digital workflow now incorporates navigation systems for both surgical and non-surgical endodontic procedures, primarily employing two techniques: static navigation and dynamic navigation [1-3]. Dynamic navigation, a computer-guided technology initially developed for precise and real-time planning in oral implantology, utilizes cameras and tracking devices attached to the handpiece and the patient. The system continuously compares the access path using software on the CBCT images, providing the clinician with information related to the milling path, which is visually displayed on a monitor [4].
Dynamic navigation systems (DNSs) have emerged as valuable tools in endodontics, finding application in various procedures, including the management of obliterated canals, post removal, and EM [2, 5-7]. A key advantage of DNS over static navigation is the elimination of the need for guide fabrication, enabling faster patient treatment [7]. Static guides, on the other hand, can pose challenges in accessing posterior regions, particularly when interocclusal space is limited [5]. Additionally, static guides can increase the risk of bone overheating due to inadequate irrigation, among other potential complications [2, 8].
The DNS uses instruments that help to perform more precise procedures at different surgical stages. For example, during osteotomy, it allows for a smaller access, which favors the repair process. This case report documented EM in a mandibular first molar using the Navident® DNS (ClaroNav, Toronto, Canada), applying the cortical window technique. Clinical and CBCT follow-up at 21 months showed a successful outcome in periapical healing.
CASE REPORT
Patient Presentation
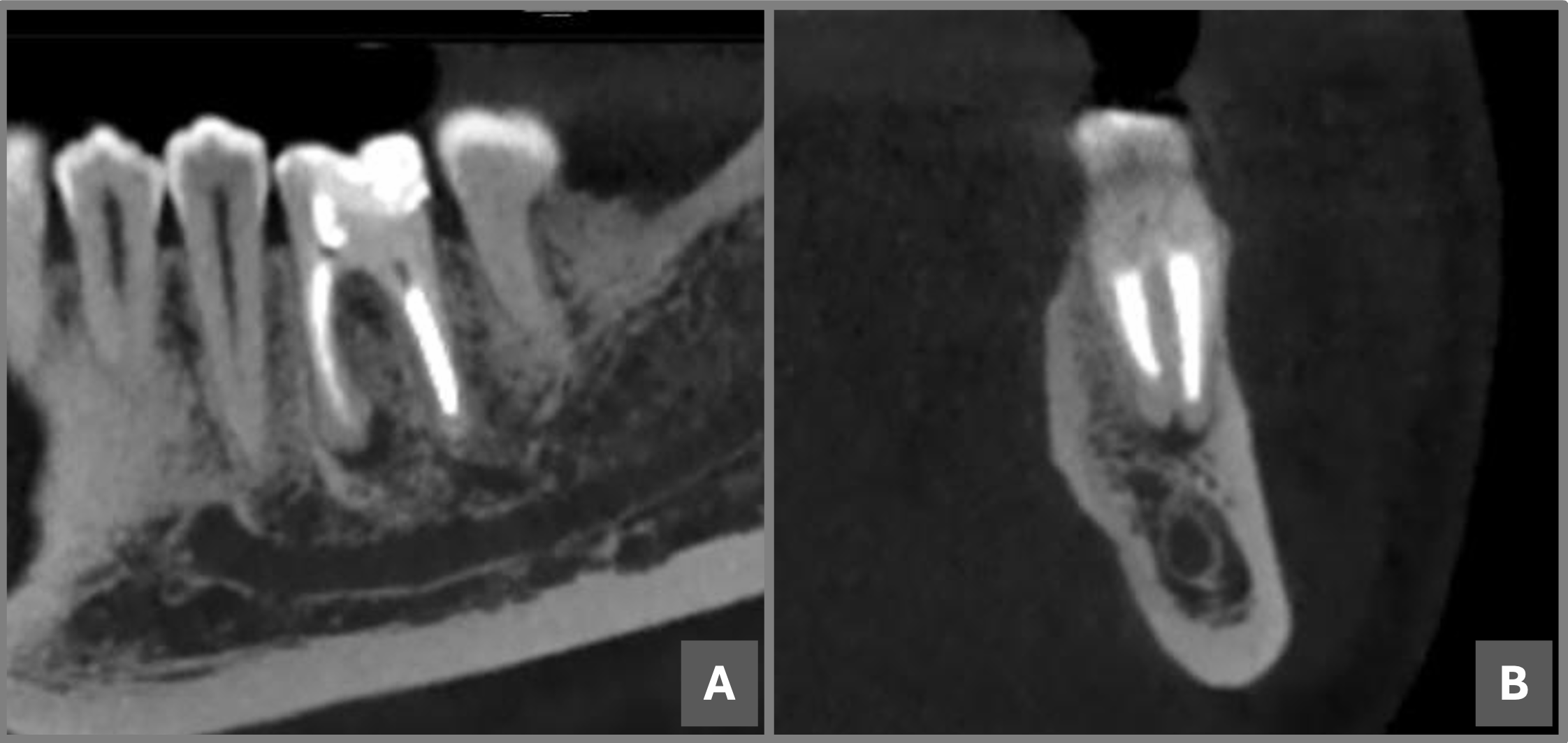
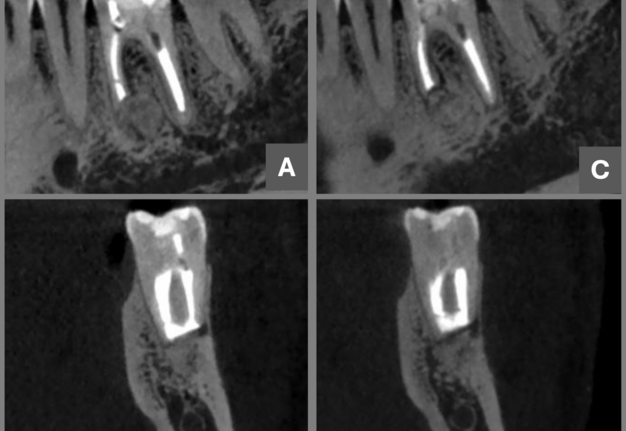
A 36-year-old male with no significant medical history presented with chief complaint of pain on chewing in the lower left quadrant. Clinical examination revealed positive vertical percussion test on tooth #36 (i.e., lower left first molar), negative palpation, physiological mobility, and normal periodontal probing depths. No swelling or sinus tract was evident. CBCT analysis (Myray, Hyperion X9 tomograph, 75 microns, 6x4 window, Imola [BO], Italy) revealed an adequate coronal restoration, along with a previous endodontic treatment performed one year ago, where the mesiolingual canal was underfilled, while the mesiobuccal and distal canals were well obturated. A hypodense periapical area was identified in the mesial root (Fig 1), accompanied by a 4 mm diameter periapical lesion. The buccal cortical bone was intact, with a thickness of 5 mm to the root apex. Based on these findings, the tooth was diagnosed as previously treated with symptomatic apical periodontitis, classified according to the periapical index (PAI) CBCT PAI 3E [9].
Surgical Procedure
Preoperative Planning and Anesthesia
Pre-surgical Planning:
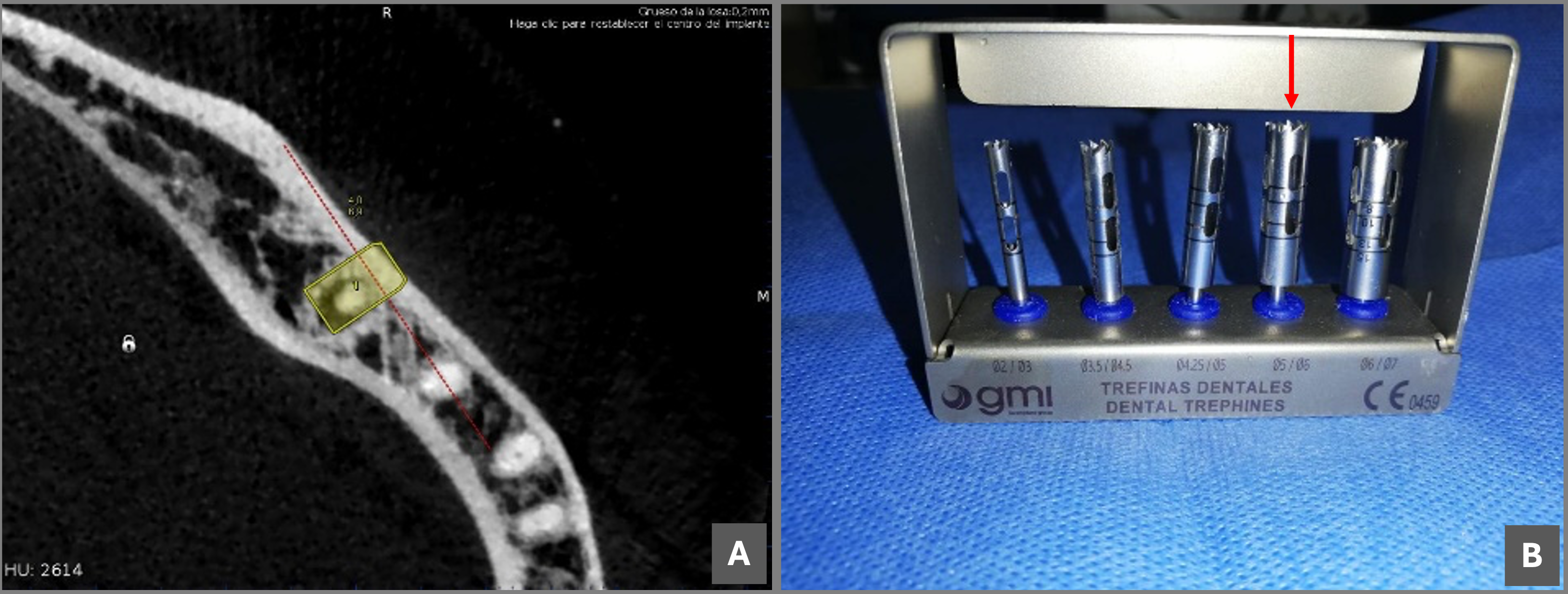
The surgical procedure commenced after obtaining informed consent and explaining treatment options. The Digital Imaging and Communications in Medicine (DICOM) data from the CBCT scan was imported into the Navident® software for meticulous surgical planning (Fig 2A). The planned angulation was set at 0-10 degrees relative to the tooth's longitudinal axis, as recommended by some studies [5].
Pre-operative Preparation:
Before surgery, a thorough 60-second rinse with 0.12% chlorhexidine solution (PerioGard®, Colgate-Palmolive, Anchieta, Brazil) was performed for oral disinfection. Local anesthesia was achieved using 2 cartridges (3,6 mL) of lidocaine 2% with epinephrine 1:80,000 (Newcaína, New Stetic, Guarne, Colombia). The anesthetic technique involved an inferior alveolar nerve block and buccal infiltration. This ensures adequate pain control throughout the surgery by blocking the nerve that supplies sensation to the lower jaw and infiltrating the surrounding tissue with an anesthetic.
Surgical Technique
A meticulous submarginal incision with a scalloped margin was placed, followed by a full-thickness flap (mucoperiosteal) elevation for optimal visualization and surgical field access. Mesial and distal releasing incisions were employed to facilitate exposure of the intact cortical bone and allow for adequate flap mobility.
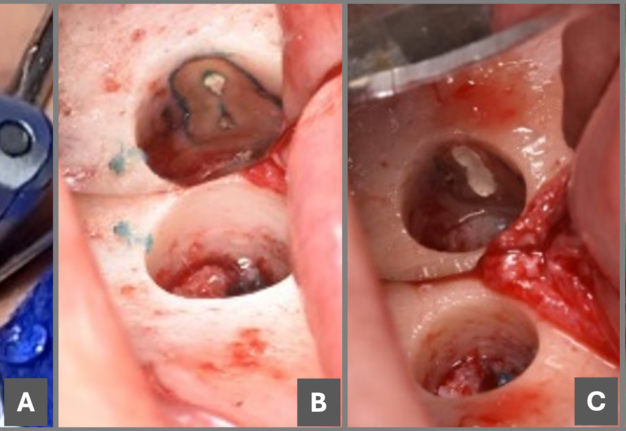
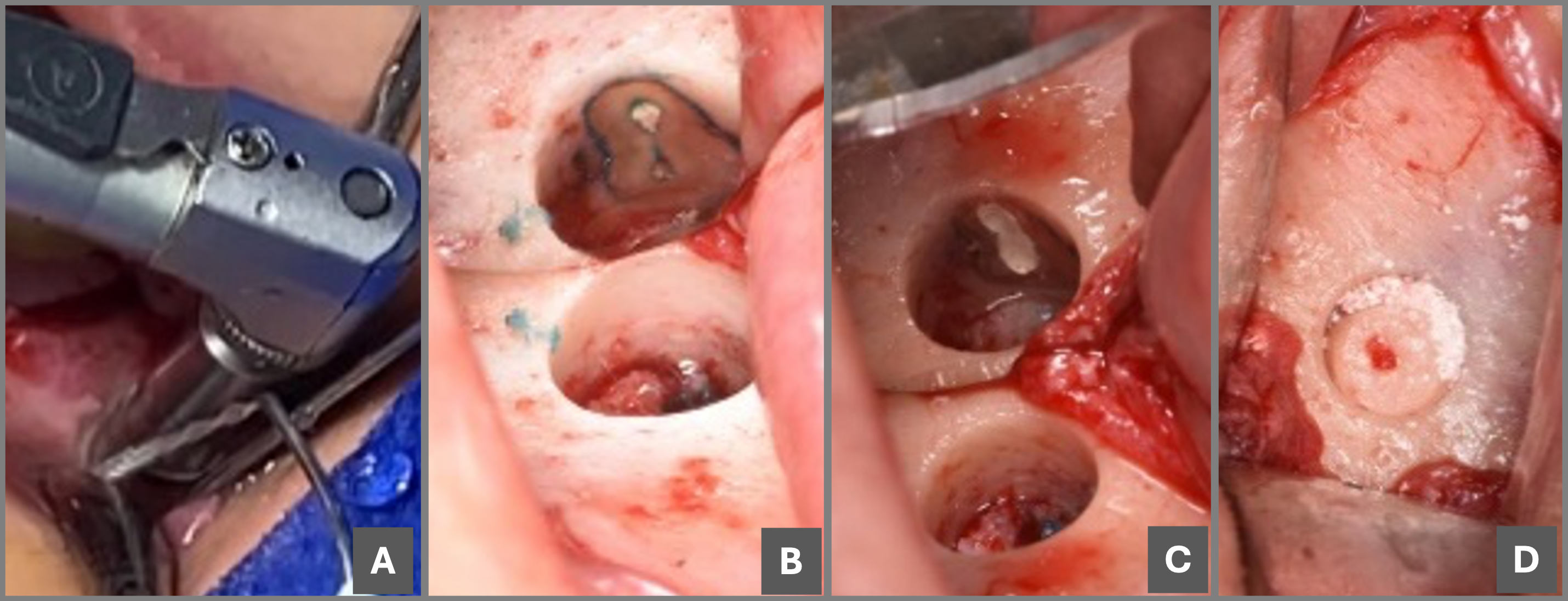
Utilizing the DNS and a 5 mm diameter trephine bur (Global Medical Implants [GMI], Lleida, Spain) attached to a contra-angle handpiece (NSK Brasil, Sao Paulo, Brazil) (Fig 2B), an osteotomy was performed at a speed of 10.000 revolutions per minute (rpm) under continuous saline irrigation for cooling and debris removal (Fig 3A). The DNS precisely guided the trephine bur, ensuring creation of a well-defined bone window and simultaneous apicectomy at the pre-planned angulation of 0 degrees relative to the tooth's longitudinal axis. The bone fragment was carefully retrieved and placed in a sterile container with saline solution for potential grafting. The apical root segment, along with the associated periapical lesion, was meticulously removed with microsurgical instruments under high magnification.
The retropreparation cavity was subsequently stained with methylene blue (Disanfer, Bogotá, Colombia) to enhance visualization of the root canal orifice and facilitate precise cavity preparation (Fig 3B). Ultrasonic diamond tips (E30LD-S, NSK, Nakanishi, Japan) were employed in conjunction with the Biosonic S1 ultrasonic unit (Coltene Whaledent, Altstätten, Switzerland) for efficient and minimally invasive cavity shaping. Continuous saline irrigation was maintained throughout the procedure to ensure cooling and debris removal, followed by thorough drying with sterile paper points (New Stetic S.A., Guarne, Colombia).
Retrograde obturation of the prepared cavity was performed using BIO-C® Repair (Angelus, Londrina, Brazil) to create a hermetic seal and prevent bacterial leakage (Fig 3C). The carefully retrieved bone fragment was stabilized within the defect using 0.5 grams of xenograft bone with a particle size range of 300 to 600 microns (Biomod 3Biomat S.A.S, Bogotá, Colombia) to promote bone healing (Fig 3D). The mucoperiosteal flap was meticulously repositioned and sutured with 5-0 Dafilon sutures (B. Braun, Tuttlingen, Germany) for tension-free closure.
The entire surgical procedure was performed under the magnification of a surgical microscope OMS2350 (Zumax Medical, Suzhou, China) to ensure optimal visualization, precise handling of instruments, and meticulous attention to detail.
Postoperative Care and Follow-up
To prevent potential infections and promote healing, the patient was prescribed a regimen of Amoxal 500 mg capsules (GlaxoSmithKline [GSK], London, England) one capsule every 8 hours for 5 days, Anexia 120 mg tablets (Tecnoquímicas S.A., Cali, Colombia) one tablet daily, and a 0.12% chlorhexidine mouthwash twice daily. Additionally, topical application of fitostimoline gel oral (Euroetika S.A.S, Bogotá, Colombia) was recommended to promote healing.
The sutures were carefully removed 7 days following the procedure. Follow-up appointments were scheduled at 6, 12, and 21 months to assess healing and ensure optimal outcomes. CBCT scans obtained at these follow-up visits revealed complete periapical healing (Fig 4), and the patient remained asymptomatic throughout the follow-up period.
DISCUSSION
In the presented case, guided EM emerged as the preferred treatment approach due to the low likelihood of successful retreatment via an orthograde technique. This decision aimed to circumvent the potential risks associated with adverse events during non-surgical endodontic retreatment, particularly root perforation in the danger zone. By employing EM, conservative management of the furcation area was achieved, an area particularly susceptible to stripping-type perforations [10, 11].
DNS stands as a novel technology that significantly enhances precision during microsurgical endodontic procedures. It serves as a real-time guide for instrument orientation, fostering the protection of adjacent anatomical structures [6]. DNS enables a conservative approach during osteotomy, particularly in cases where cortical bone fenestration is absent or when the cortical thickness hinders access to the root apex. This conservative approach positively impacts bone healing time, as evidenced by the successful outcome in the presented case. However, DNS has drawbacks, including its high acquisition cost and the substantial space requirement due to the equipment's size [12]. Additionally, it presents a steeper learning curve than traditional techniques or static guides, demanding operator calibration, manual dexterity, and exceptional hand-eye coordination [4].
Currently, several systems facilitate a more conservative and precise osteotomy phase during EM. One such system is the piezoelectric system, equipped with diverse tips that offer protection against nerve structure damage and minimize bleeding, enhancing visibility during the procedure [13-15]. Another option is the use of trephines, available in various diameters and lengths. Trephines allow for the preservation of the intact bone block that is removed, enabling its subsequent repositioning and, if necessary, fixation before flap replacement [12, 16].
Research suggests that computer-assisted static navigation techniques planned with trephines offer a cylindrical geometry that helps prevent unwanted deviations during osteotomy. This can result in greater accuracy in locating the root apex [17]. This technique, known as the "cortical window," facilitates faster healing, considering autologous bone's osteogenic, osteoinductive, and osteoconductive potential [14, 15]. Given the advantages mentioned above and others reported in the literature, the cortical window technique guided by DNS using a trephine was employed in the presented case. The primary objective was to preserve the bone structure, maintain the integrity of the vestibular cortical bone, facilitate access to the root to be treated, and enable successful apicectomy [12, 14, 18].
CONCLUSION
This case report demonstrates the successful application of dynamic navigation system (DNS) combined with the cortical window technique using a trephine for endodontic microsurgery (EM) of a mandibular molar with a periapical lesion and intact buccal cortical bone. This minimally invasive approach facilitated precise osteotomy, root apex access, and retrograde filling, leading to successful periapical healing at the 21-month follow-up as confirmed by cone-beam computed tomography (CBCT).
Key Advantages of the Technique:
-
Enhanced Precision: DNS provides real-time guidance, minimizing the risk of iatrogenic complications during osteotomy and protecting vital structures.
-
Conservative Approach: The cortical window technique allows for a smaller access cavity, preserving bone structure and promoting faster healing.
-
Autologous Bone Grafting: Repositioning the retrieved bone fragment promotes osteoconduction and facilitates bone regeneration in the defect area.
Future Directions:
While DNS offers significant benefits, further research is needed to evaluate its long-term cost-effectiveness compared to traditional techniques. Additionally, advancements in technology and user interface design can potentially reduce the learning curve associated with DNS.
Overall Significance:
This case report highlights the potential of DNS-guided EM with the cortical window technique as a predictable and minimally invasive treatment option for managing complex endodontic cases with limited surgical access. This approach offers a promising future for improving surgical outcomes and patient care in EM.
AUTHOR CONTRIBUTIONS
Conceptualization, G.A.C. and O.E.Z.; methodology, G.A.C., O.E.Z., and P.A.E-V.; software, G.A.C.; validation, G.A.C.; formal analysis, G.A.C.; investigation, G.A.C.; resources, G.A.C., O.E.Z., S.A.R-M., and P.A.E-V.; data curation, G.A.C., O.E.Z., S.A.R-M., and P.A.E-V.; writing—original draft preparation, G.A.C., O.E.Z., and P.A.E-V.; writing—review and editing, G.A.C., O.E.Z., S.A.R-M., and P.A.E-V.; visualization, G.A.C., O.E.Z., and P.A.E-V.; supervision, G.A.C., O.E.Z., and P.A.E-V.; project administration, G.A.C., O.E.Z., and P.A.E-V. All authors have read and agreed to the published version of the manuscript.
FUNDING
This research received no external funding.
INSTITUTIONAL REVIEW BOARD STATEMENT
Not applicable.
INFORMED CONSENT STATEMENT
Informed consent was obtained from the patient for the publication of this study.
DATA AVAILABILITY STATEMENT
Not applicable.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
ORCID
Gustavo A. Castillo: https://orcid.org/0009-0002-0534-9941
Silvia A. Restrepo-Méndez: https://orcid.org/0009-0005-6021-2229
Oscar E. Zuluaga: https://orcid.org/0009-0009-0687-3295
Paola A. Escobar-Villegas: https://orcid.org/0000-0003-0703-0475
REFERENCES (18)
-
Tang W, Jiang H. Comparison of static and dynamic navigation in root end resection performed by experienced and inexperienced pperators: an in vitro study. J Endod. 2023;49(3):294-300.https://doi.org/10.1016/j.joen.2022.11.016
-
D GT, Saxena P, Gupta S. Static vs. dynamic navigation for endodontic microsurgery - A comparative review [published correction appears in J Oral Biol Craniofac Res. 2024 Jul-Aug;14(4):358-359. https://doi.org/10.1016/j.jobcr.2024.05.010 ]. J Oral Biol Craniofac Res. 2022;12(4):410-412. https://doi.org/10.1016/j.jobcr.2022.04.010
-
Ribeiro D, Reis E, Marques JA, et al. Guided endodontics: static vs. dynamic computer-aided techniques—a literature review. J Pers Med. 2022;12(9):1516. https://doi.org/10.3390/jpm12091516
-
Vasudevan A, Santosh SS, Selvakumar RJ, et al. Dynamic navigation in guided endodontics - a systematic review. Eur Endod J. 2022;7(2):81-91. https://doi.org/10.14744/eej.2022.96168
-
Villa-Machado PA, Restrepo-Restrepo FA, Sousa-Dias H, Tobón-Arroyave SI. Application of computer-assisted dynamic navigation in complex root canal treatments: report of two cases of calcified canals. Aust Endod J. 2022;48(1):187-196. https://doi.org/10.1111/aej.12614
-
Aldahmash SA, Price JB, Mostoufi B, et al. Real-time 3-dimensional dynamic navigation system in endodontic microsurgery: a cadaver study. J Endod. 2023;48(7):922-929. https://doi.org/10.1016/j.joen.2022.04.012
-
Martinho FC, Griffin IL, Corazza BJM. Current applications of dynamic navigation system in endodontics: a scoping review. Eur J Dent. 2023;17(03):569-586. https://doi.org/10.1055/s-0042-1749361
-
Dianat O, Nosrat A, Mostoufi B, et al. Accuracy and efficiency of guided root-end resection using a dynamic navigation system: a human cadaver study. Int Endod J. 2021;54(5):793-801. https://doi.org/10.1111/iej.13466
-
Estrela C, Bueno MR, Azevedo BC, et al. A new periapical index based on cone beam computed tomography. J Endod. 2008;34(11):1325-1331. https://doi.org/10.1016/j.joen.2008.08.013
-
Zanza A, Reda R, Testarelli L. Endodontic orthograde retreatments: challenges and solutions. Clin Cosmet Investig Dent. 2023;15:245-265. https://doi.org/10.2147/ccide.s397835
-
Wei X, Du Y, Zhou X, et al. Expert consensus on digital guided therapy for endodontic diseases. Int J Oral Sci. 2023;15(1):54. https://doi.org/10.1038/s41368-023-00261-0
-
Antal M, Nagy E, Sanyó L, Braunitzer G. Digitally planned root end surgery with static guide and custom trephine burs: a case report. Int J Med Robot Comput Assist Surg. 2020;16(4):e2115. https://doi.org/10.1002/rcs.2115
-
Kim U, Kim S, Kim E. The application of “bone window technique” using piezoelectric saws and a CAD/CAM-guided surgical stent in endodontic microsurgery on a mandibular molar case. Restor Dent Endod. 2020;45(3):e27. https://doi.org/10.5395/rde.2020.45.e27
-
Fernández-Grisales R, Rojas W, Berruecos-Orozco C. Piezoelectric endodontic microsurgery with modified cortical window technique: a case report. J Endod Microsurg. 2023;2:34-40. https://doi.org/10.23999/jem.2023.2.4
-
Floratos S, Molonis V, Tsolakis A, et al. Bone window technique in endodontic microsurgery – report of two cases. J Endod Microsurg. 2023;2:24-33. https://doi.org/10.23999/jem.2023.2.3
-
Antal M, Nagy E, Braunitzer G, et al. Accuracy and clinical safety of guided root end resection with a trephine: a case series. Head Face Med. 2019;15(1):30. https://doi.org/10.1186/s13005-019-0214-8
-
Madroño EC, Torres PR, Oussama S, et al. A comparative analysis of the piezoelectric ultrasonic appliance and trephine bur for apical location: an in vitro study. J Pers Med. 2021;11(10):1034. https://doi.org/10.3390/jpm11101034
-
Lee SM, Yu YH, Wang Y, et al. The application of “bone window” technique in endodontic microsurgery. J Endod. 2020;46(6):872-880. https://doi.org/10.1016/j.joen.2020.02.009
ABSTRACT IN UKRAINIAN (PDF). АНОТАЦІЯ
Останні досягнення в ендодонтичній хірургії значно покращили результати завдяки вдосконаленій технології, включаючи цифрове планування, конусно-променеву комп’ютерну томографію (КПКТ) та операційні мікроскопи. Інтеграція динамічних навігаційних систем (ДНС) особливо змінила ендодонтичну мікрохірургію (EM), забезпечуючи вказівки в реальному часі та точність. У цьому звіті досліджується застосування ДНС у клінічному випадку EM, що включає перший моляр нижньої щелепи з симптоматичним апікальним періодонтитом. Пацієнт чоловічої статі 36 років звернувся зі скаргами на біль при жуванні у лівому нижньому квадранті. Рентгенографія та КПКТ виявили недостатньо заповнений мезіолінгвальний кореневий канал і періапікальне ураження. Під час хірургічної процедури використовувалася ДНС для точної остеотомії та апікоектомії за допомогою системи Navident® і включала методику "кортикального вікна". Післяопераційний догляд включав антибіотикотерапію та контрольні огляди, що продемонструвало успішне періапікальне загоєння через 21 місяць. Технологія ДНС значно підвищує точність і консервативність ЕМ, дозволяючи надавати вказівки в реальному часі та мінімізуючи ятрогенні ризики. Методика "кортикального вікна" в поєднанні з ДНС полегшує ефективний доступ до кореня, зберігаючи структуру кістки. Незважаючи на свої переваги, ДНС пов’язаний з високими витратами та крутою кривою навчання. Майбутні дослідження мають бути зосереджені на оцінці довгострокових клінічних результатів ДНС, покращенні зручності використання системи та дослідженні її застосування в інших ендодонтичних процедурах. Цей випадок демонструє успішне використання ДНС у поєднанні з методикою "кортикального вікна" для ЕМ, що забезпечує сприятливі клінічні результати та сприяє прискоренню загоєння. Потрібні подальші дослідження, щоб підтвердити ширшу клінічну корисність ДНС і вдосконалити її інтеграцію в повсякденну практику.
ABSTRACT IN SPANISH (PDF). RESUMEN
Los recientes avances en la cirugía endodóncica han mejorado significativamente los resultados a través de una tecnología mejorada, que incluye la planificación digital, la tomografía computarizada de haz cónico (TCHC) y los microscopios quirúrgicos. La integración de los sistemas de navegación dinámica (SND) ha transformado particularmente la microcirugía endodóncica (ME) al proporcionar guía y precisión en tiempo real. Este informe de caso explora la aplicación de DNS en un caso clínico de ME que involucraba un primer molar mandibular con periodontitis apical sintomática. Un paciente masculino de 36 años presentó dolor masticatorio en el cuadrante inferior izquierdo. Las evaluaciones radiográficas y TCHC revelaron un conducto mesiolingual insuficientemente obturado y una lesión periapical. El procedimiento quirúrgico utilizó SND para una osteotomía y apicectomía precisas, guiadas por el sistema Navident® e incorporando la técnica de ventana cortical. El cuidado posoperatorio incluyó terapia con antibióticos y citas de seguimiento, demostrando una curación periapical exitosa a los 21 meses. La tecnología SND mejora significativamente la precisión y el carácter conservador en la ME, lo que permite una guía en tiempo real y minimiza los riesgos iatrogénicos. La técnica de ventana cortical, combinada con SND, facilita el acceso eficaz a la raíz al tiempo que preserva la estructura ósea. A pesar de sus ventajas, SND está asociada a altos costos y una curva de aprendizaje pronunciada. Las investigaciones futuras deben centrarse en evaluar los resultados clínicos a largo plazo de SND, mejorar la usabilidad del sistema y explorar sus aplicaciones en otros procedimientos endodóncicos. Este informe de caso demuestra el uso exitoso de SND junto con la técnica de ventana cortical para ME, logrando resultados clínicos favorables y promoviendo una curación acelerada. Se necesitan más estudios para validar la utilidad clínica más amplia de SND y refinar su integración en la práctica de rutina.