Piezoelectric Endodontic Microsurgery with Modified Cortical Window Technique: A Case Report
September 13, 2023
J Endod Microsurg. 2023;2: 34-40.
Under a Creative Commons license
HOW TO CITE THIS ARTICLE (AMA Referencing)
Fernández-Grisales R, Rojas WJ, Berruecos-Orozco C. Piezoelectric endodontic microsurgery with modified cortical window technique: a case report. J Endod Microsurg. 2023;2:34-40. https://doi.org/10.23999/jem.2023.2.4
National Repository of Academic Texts
https://nrat.ukrintei.ua/searchdoc/2023U000228 (in English). https://nrat.ukrintei.ua/searchdoc/2023U000228 (in Ukrainian)
ABSTRACT
Osteotomy in endodontic microsurgery for teeth with periapical lesions which have not perforated the cortical plate can be a complex procedure especially if anatomical structures such as the mental nerve are close to the area of surgical intervention. For such cases, the cortical bone window technique is an excellent option to access the operating field, preserving the cortical bone and avoiding the use of other bone regeneration materials. The present case documented the use of the cortical bone window technique with a modification, due to the proximity of the mental nerve to approach a persistent periapical lesion of a mandibular second premolar with previous endodontic treatment. Cone beam computed tomography (CBCT) and intraoral scanning were used for planning and elaboration of a navigation guide for surgical procedure. The clinical and radiographic 5-month follow-up with periapical radiography and CBCT revealed a favorable outcome, with an asymptomatic patient and an advanced healing process at the previous periapical lesion site.
KEY WORDS
Bone window; cone beam computed tomography; endodontic microsurgery; graft; osteotomy; piezoelectric surgery
INTRODUCTION
Endodontic microsurgery (EM) is a treatment option for persistent apical periodontitis in endodontically treated teeth where non-surgical retreatment is not deemed not to be feasible [1, 2]. EM has high success rates; 96.8% and 91.5% at 1-year and 5–7 year follow-ups, respectively [3]. Previously, conventional endodontic surgery used periapical radiography for case planning and follow-up and high-speed handpieces for osteotomy and apical resection [4, 5]. Currently, EM is performed with the aid of operating microscopes (OMs), cone beam computed tomography (CBCT), ultrasonics and piezoelectric devices to manage the apical root canal anatomy and surrounding tissues and to improve treatment outcomes [6].
In the presence of bone fenestration, access to the root apex is easier to identify as it is already created by the periapical lesion (PL). However, when the lesion is confined within an intact, thick buccal cortical bone, it may be difficult to locate the root apex, resulting in potentially an extensive osteotomy. This is particularly true if it is performed freehand with a high-speed handpiece [7]. In such cases, piezoelectric-guided EM with the “cortical bone window” technique has been proposed as a more conservative and precise alternative to osteotomy and apicoectomy by use of a bur [8–10]. To carry out this procedure, three elements should be considered: DICOM (Digital Imaging and Communications in Medicine) files derived from CBCT, STL (‘Standard Triangle Language’ or ‘stereolithography’) files derived from intraoral scanning, and a software capable of integrating these files to obtain a digital surgical guide, which is later printed for intraoral use [10, 11]. Thus, the osteotomy is performed on the guide’s demarcation with the saw-type inserts coupled to the piezoelectric device. Once the bone block is removed, the apicoectomy, retro-preparation, and retro-filling procedures follow. Finally, the bone block is placed in its original position, acting as an autograft with osteogenecity, osteoinductivity, and osteoconductivity features [11, 12].
In cases where the osteotomy/apicoectomy area is close to critical anatomical structures, such as the inferior alveolar and mental nerves the “cortical bone window” technique can be modified to avoid nerve damage [10, 13–15]. The present case report describes a piezoelectric-guided EM with the modified “cortical bone window” (MCBW) technique in a mandibular second premolar with persistent apical periodontitis, whose apex was in proximity to the mental nerve.
CASE REPORT
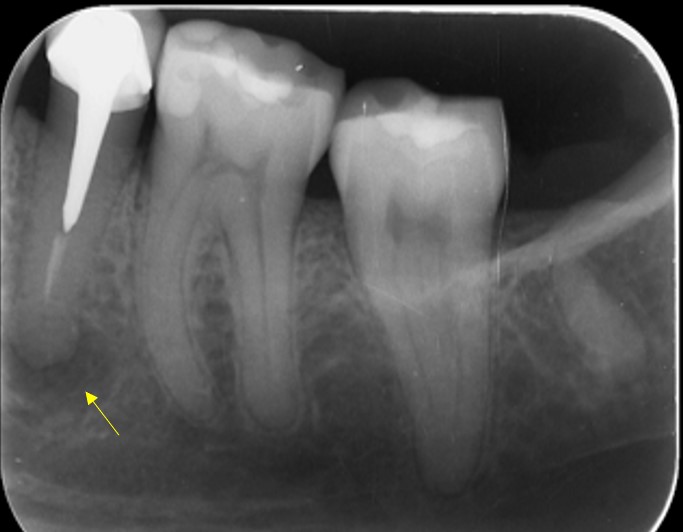
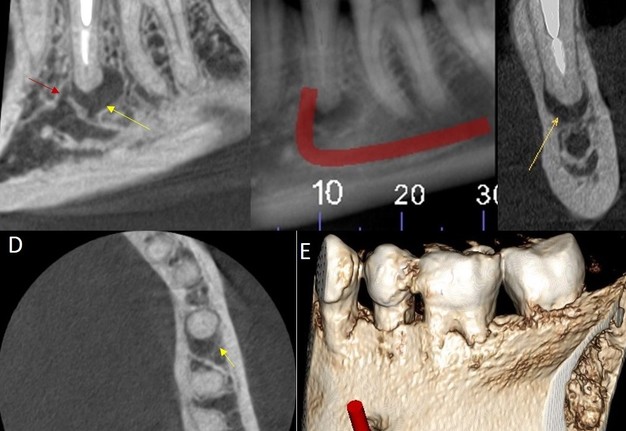
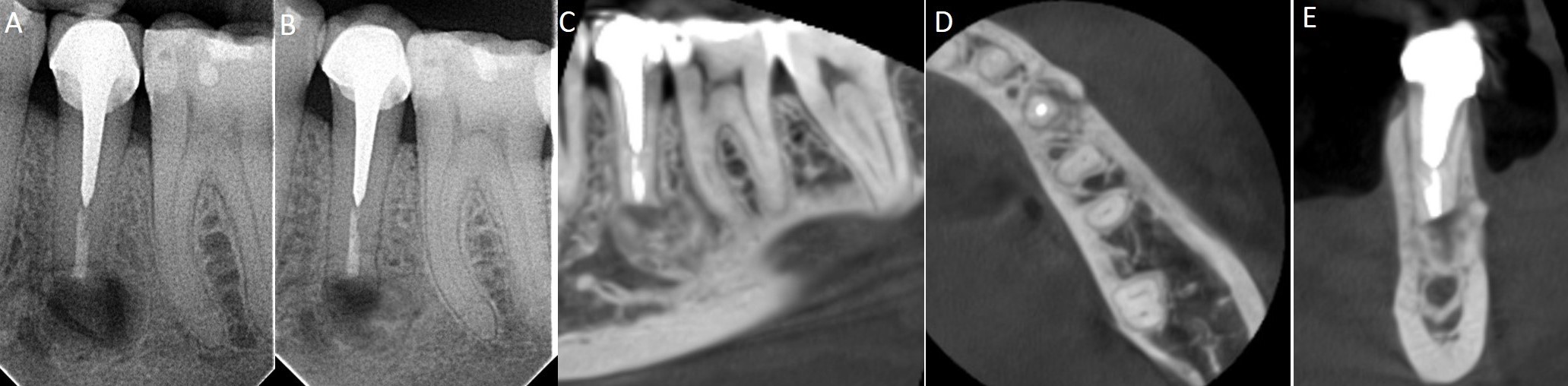
A 39-year-old woman with non-contributory medical history was referred by a prosthodontist for endodontic management of the left mandibular second premolar (tooth #35). The clinical examination revealed an all-ceramic crown with good marginal adaptation, ≤3 mm periodontal probing, grade I mobility, and pain on vertical percussion. Digital periapical radiography (DPR) (Gendex VISUALIX EHD, Hatfield, Pennsylvania, USA) (Fig 1) and CBCT (Planmeca ProMax 3D Classic, Planmeca®, Helsinki, Finland) operating at 90 kVp, 16 mA, field of view 50 × 40 mm, voxel size 75 μm, 16 bits, and 15 sec exposure (Fig 2A–E), revealed a single root canal with an intraradicular post, an endodontic filling of adequate density but short of the radiographic apex, and a visible root canal lumen in the apical third. In addition, a periapical radiolucent image was observed close to the mental foramen. Based on the above findings, the diagnosis was an endodontically treated tooth with symptomatic chronic apical periodontitis. The treatment plan included guided EM.
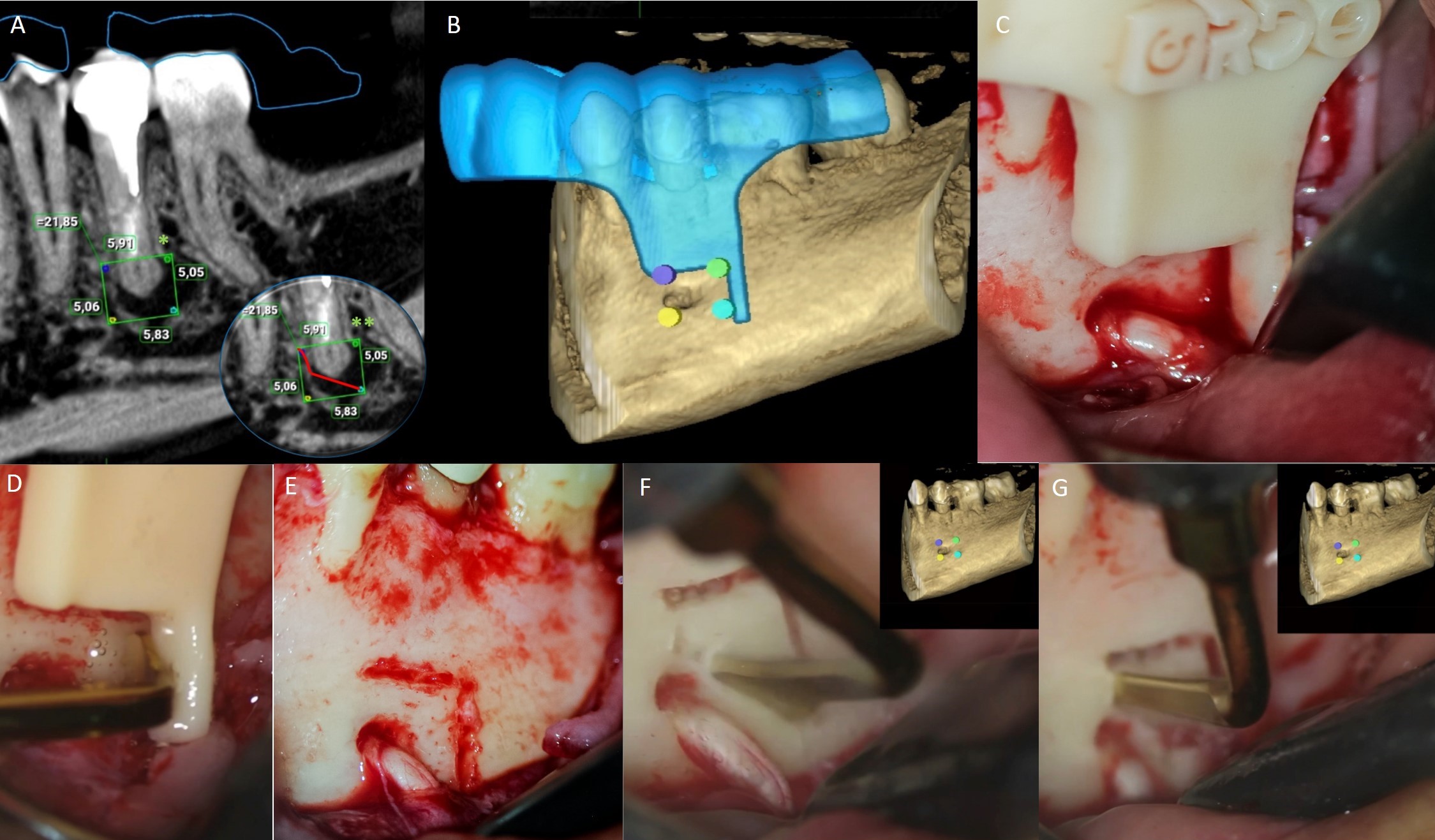
FIGURE 2. Cone beam computed tomography of tooth #35. (A, B) (sagittal plane), the yellow arrow shows the periapical lesion, and the red arrow shows the mental foramen. Also, the trajectory of the mental foramen is indicated. (C, D) (coronal and axial sections, respectively), the yellow arrow shows the periapical lesion between the buccal and lingual cortical bone. (E) volumetric reconstruction showing the mental foramen close to the apex of tooth #20.
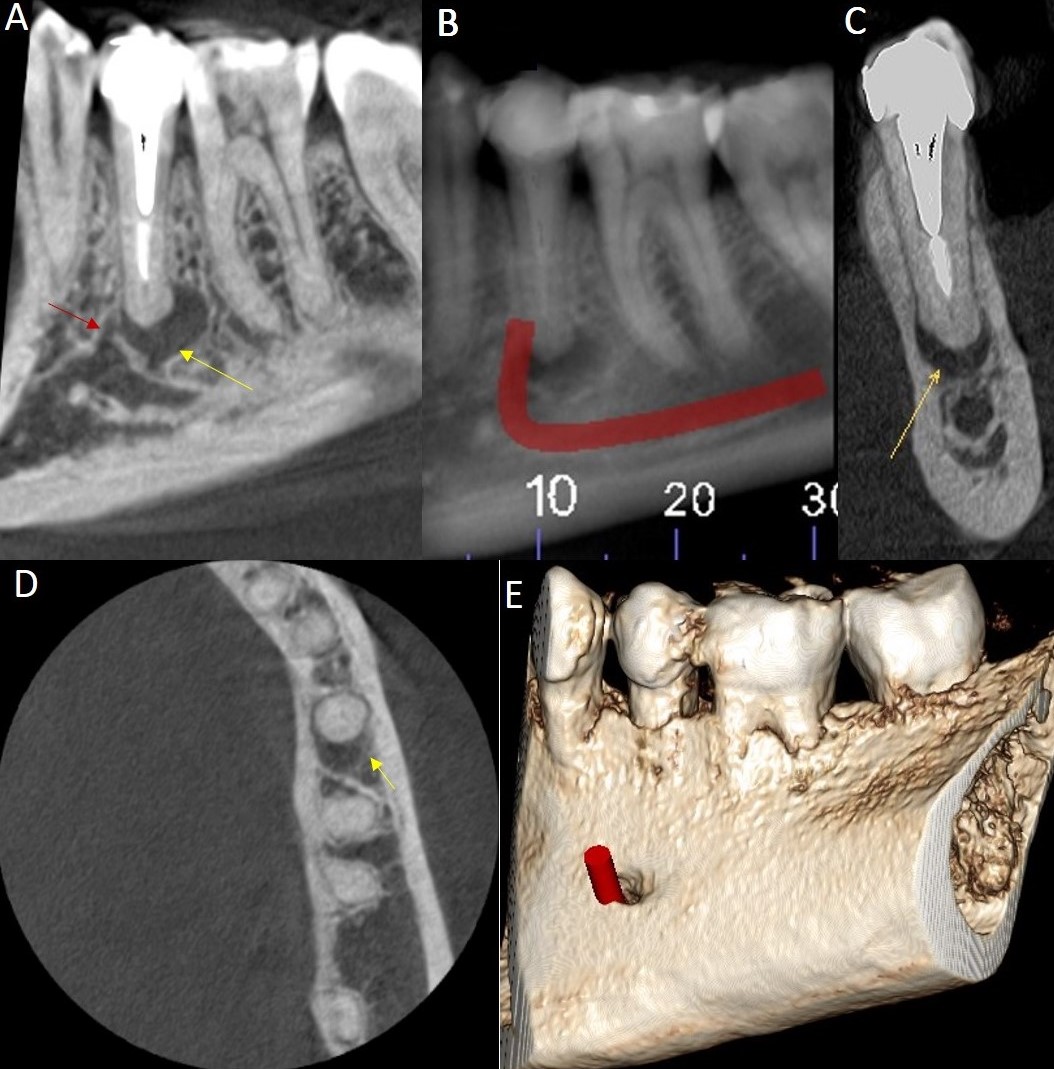
In order to plan the guide, DICOM and STL files were obtained from the CBCT and intraoral scan (3Shape Trios3, TR3, 3Shape A/S, Copenhagen, Denmark) respectively, and integrated into the Romexis software (version 3.8.2.R Planmeca, Helsinki, Finland) for the design and construction of a 3D printed (Eden260VS Dental Advantage, Stratasys Ltd.), resin-supported dento-osseous surgical guide (MED610 by Stratasys Ltd., Eden Prairie, MN, USA), which was utilized during the osteotomy ensuring mental nerve integrity (Fig 3A–B). An operating microscope (ZUMAX OMS 2350, Zumax Medical, Suzhou New District, China) and piezoelectric bone surgery system (Woodpecker Ultrasurgic Touch unit, Guilin Woodpecker Medical Instrument Co. LTD, Guilin, Guangxi, China) were also used during the surgical procedure.
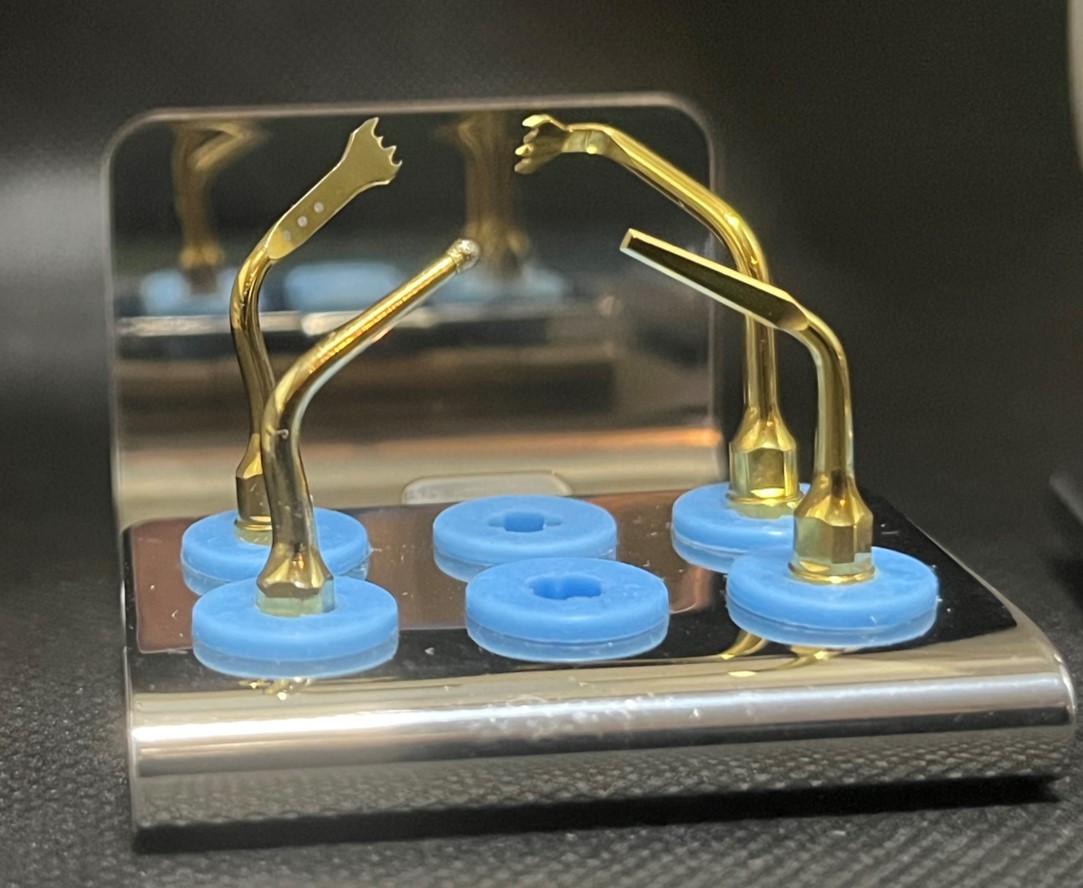
FIGURE 3. Tomographic and clinical sequence of the design and performance of the modified “cortical bone window” technique on tooth #35. (A) sagittal plane. One superscript asterisk (*) shows the typical rectangular design of the “cortical window” technique. Two superscript asterisks (**) show the design of the modified “cortical bone window” technique. (B) digital surgical guide design for the modified “cortical window” technique. (C) clinical positioning of the surgical guide. (D) US1L piezoelectric tip cutting with the surgical guide in position. (E) partial design of the modified “cortical bone window” technique. (F, G) US1 and UC1 piezoelectric tips, respectively, were used to complete the modified “cortical window” technique.
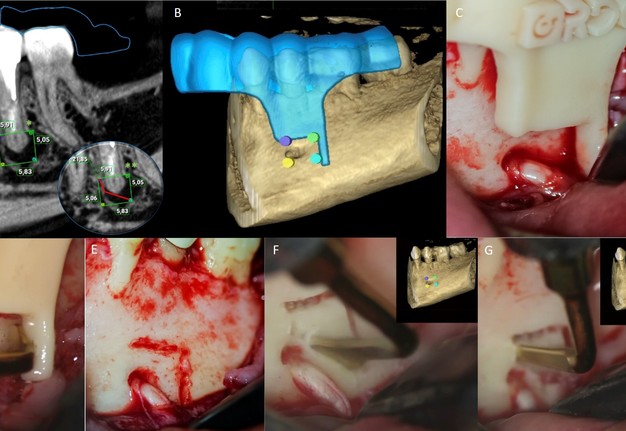
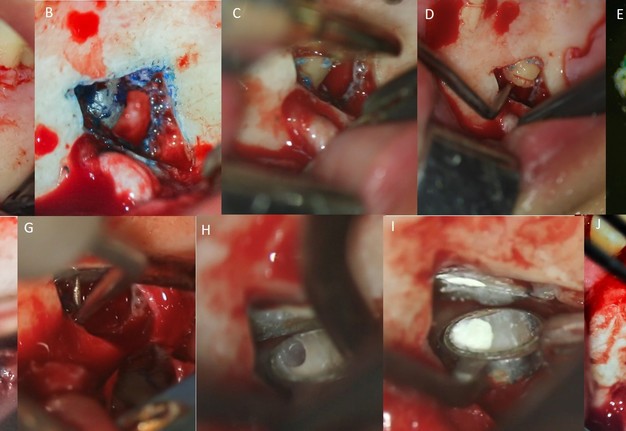
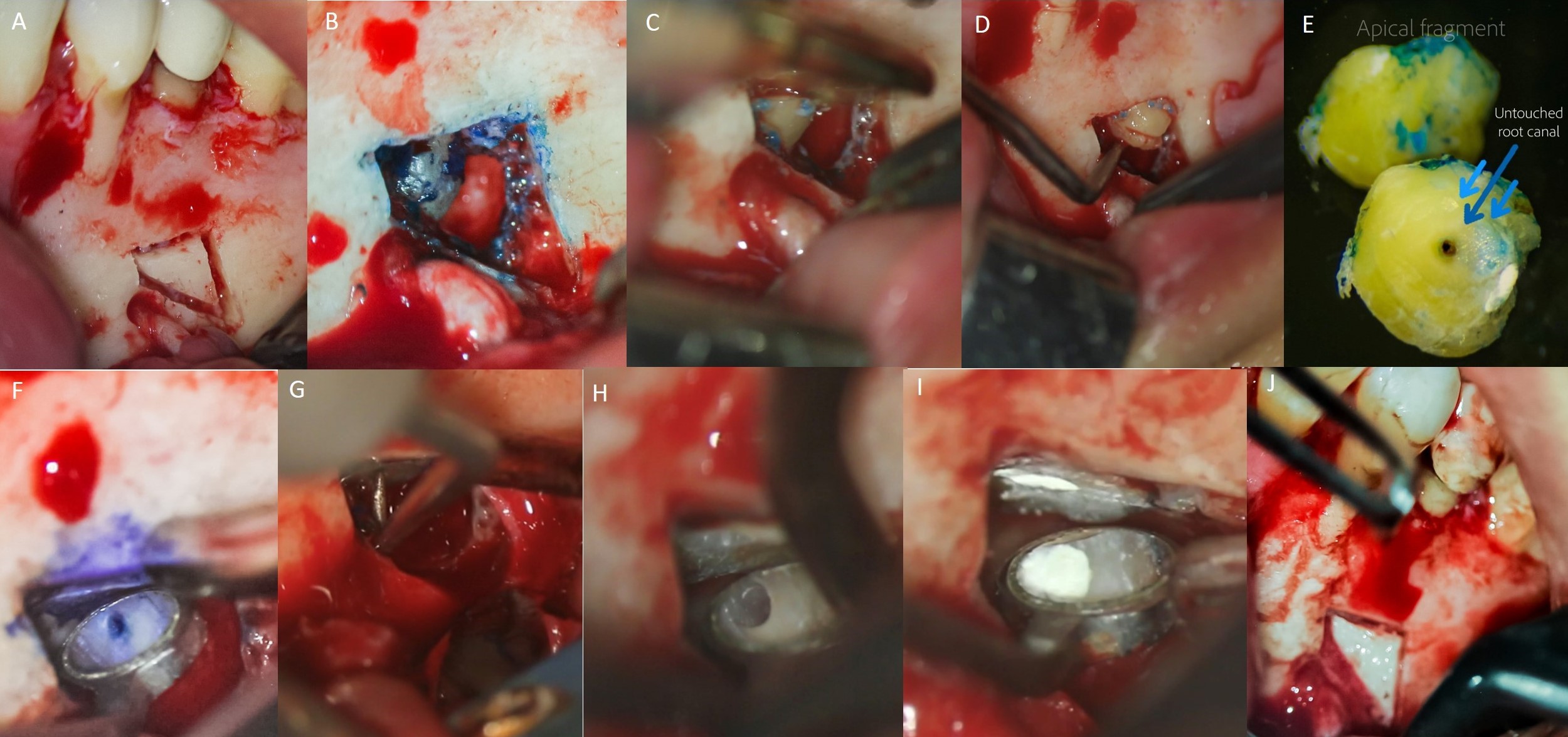
Before the procedure, the patient was asked to rinse with 0,12% chlorhexidine (Clorhexol, Farpag, Bogotá, Colombia) for 2 minutes. 2% lidocaine with 1:80.000 epinephrine (New Stetic, Guarne, Colombia) local anesthesia was applied with 3 carpules to anesthetize inferior alveolar nerve and 1 carpule to anesthetize mental nerve. A full-thickness triangular flap with released on the distal aspect of tooth #33 and an intrasulcular incision extending to the distal aspect of tooth #36 was made. Once the bone surface was exposed, the surgical guide was positioned, and the cutting procedure of the MCBW technique was performed (Fig 3C–G) using the US1L, US1R, US1, and UC1 tip (Fig 4), coupled to the piezoelectric device (Ultrasurgic touch, Woodpecker Medical Instrument Co. LTD, Guilin, Guangxi, China), in bone mode, power level 4 and water level 5 on the screen, with short movements and sustained pressure on the bone surface. Subsequently, a triangular cortical window was dislodged using a mini Buser periosteal elevator (Salvin Inc, Charlotte, NC, USA). Then, the root surface was accessed (Fig 5A–B), and a 3 mm perpendicular cut apicoectomy was completed with the US3 tip, revealing the untreated apical portion of the root canal. This was confirmed with an operating microscope and the aid of methylene blue (Fig 5C–F). After curettage of the periapical inflammatory tissue, hemostasis was obtained with the use of an epinephrine pellet (RacelletTM, Ultradent, South Jordan, UT, USA), followed by the retropeparation of the apical cavity apical with a KiS 4-D ultrasonic tip (Young Specialties, Algoquin, IL, USA) (Fig 5G–H). Irrigation of the apical cavity was done with 2% chlorhexidine (ConsepsisTM, Ultradent, South Jordan, UT, USA), followed by drying with a capillary tip (Ultradent, South Jordan, UT, USA) and apical retro filling with Bio-C© Repair (Angelus, Londrina, Brazil) bioceramic reparative material (Fig 5I). Next, the RacelletÔ pellet was removed from the bone crypt, and a collagen dressing (Collatape, Zimplant, Bogotá, Colombia) was applied to help stabilize and hold the cortical window in position (Fig 5J). The flap was repositioned and secured with absorbable Vycril Plus 6-0 (Ethicon, J&J, Cincinnati, OH, USA). Finally, the patient was given post-surgical instructions of 0.12% chlorhexidine (Farpag SAS, Bogotá, Colombia) rinses and 875 mg amoxicillin BID for 7 days, and 7.5 mg meloxicam BID for 3 days. One week later, the sutures were removed, and a post-surgical DPR was taken, showing the cortical window and retro filling material in position. A 5-month follow-up with DPR and CBCT was also documented (Fig 6A–E).
FIGURE 5. Clinical sequence of endodontic microsurgery on tooth #35 with the modified “cortical bone window” technique. (A) cortical window ready to be dislodged. (B) root surface to be resected, visualized with the operating microscope at 8× and the aid of methylene blue. (C) 3 mm per cut apical resection from the root apex, using the US3 piezoelectric tip. (D) and (E), removal and inspection of the apical portion. (F) inspection of the resected tooth surface. Methylene blue shows the untreated portion of the root canal at 12× magnification. (G) ultrasound preparation of the apical cavity. (H), apical cavity after ultrasonic preparation. (I) apical cavity retro-filled with Bio-C© Repair bioceramic reparative material. (J) cortical window repositioned and stabilized prior to suturing.
FIGURE 6. Periapical radiograph and CBCT follow-up of tooth #35. (A) post-surgical digital periapical radiograph showing apical filling material and cortical window in position. Five-moth follow-up by (B) periapical radiograph and CBCT: (C) sagittal, (D) axial, and (E) coronal planes showed healing in progress.
DISCUSSION
The size of the bone defect resulting from osteotomy during endodontic surgery is associated with increased postoperative pain and inflammation and delayed bone healing [10]. Thus, the “cortical bone window” technique is an excellent alternative to preserve the integrity of the buccal cortical plate [6, 7, 12]. In this technique, the cortical window constitutes an autologous bone barrier that has been shown to be better than allografts and xenografts in terms of speed and quality of bone regeneration due to its osteogenic, osteoinductive, and osteoconductive potential [10, 16, 17]. Additionally, this technique allows potentially faster and more accurate access to the root apex, facilitating visibility of the surgical area and higher control of periapical curettage, apicoectomy, retro-preparation, and retro-filling procedures. All these conditions can help complete the technical challenges of EM which in turn may improve the outcome of EM-subjected teeth [5, 7, 18].
According to literature, the “cortical window” technique is indicated for PLs within an intact buccal cortical plate of at least 1 mm thick [10]. In the case presented here, the PL was constrained by a 1.6 mm thick cortical bone based on the CBCT, which was an indication for “cortical bone window” technique in the guided EM. However, the proximity of the PL to the mental nerve required a modification of the technique to avoid its damage. The CBCT with high resolution and small field of view allowed planning the most appropriate shape for the cortical window, which was triangular and not square, rectangular, or trapezoidal, as it is frequently designed [15]. Then, the surgical guide facilitated a precise bone cut and osteotomy utilizing the piezoelectric device. Such a procedure is more challenging to perform when done freehand.
Once the small triangular bone block was removed, the surgical site was easily accessed, and the remaining EM procedures were performed through the cortical window. In this regard, large bone defects derived from osteotomy have been associated with longer healing processes than small bone defects [6, 11, 12]. It is also important to highlight that the piezoelectric device used in this case works with a frequency between 24 and 32 kHz and constant irrigation of 40 ml/min NaCl, which ensures a safe and precise bone cut. When the device power is set to medium, the inserts do not cut into soft tissue, thus protecting nearby nerves and large blood vessels. Moreover, it causes less bleeding and maintains a physiological temperature in the cutting area due to the air-water cavitation effect, resulting in greater surgical visibility, faster bone healing, and improved patient recovery [19, 20]. This correlates with the clinical and radiographic findings of the present case, where the patient only reported a slight inflammation in the surgical area and no use of analgesics after the third postoperative day. No mental nerve paresthesia or dysesthesia were reported by the patient. The digital periapical radiograph and CBCT 5-month follow-up showed satisfactory periapical bone healing, considering the short-term follow-up available.
CONCLUSION
Incorporating CBCT, intraoral scanner, and piezoelectric device into the EM allows the planning and execution of highly complex cases and leads to successful and predictable results. The MCBW technique is an excellent alternative that provides safer and more conservative osteotomy/apicoectomy in EM cases of PLs without bone fenestration located close to critical anatomical structures such as the mental nerve.
REFERENCES (20)
-
Dioguardi M, Stellacci C, La Femina L, et al. Comparison of endodontic failures between nonsurgical retreatment and endodontic surgery: systematic review and meta-analysis with trial sequential analysis. Medicina. 2022;58(7):894. Link
-
Prada I, Mico-Munoz P, Giner-Lluesma T, et al. Influence of microbiology on endodontic failure. Literature review. Med Oral Patol Oral Cir Bucal. 2019; e364-72. Link
-
Huang S, Chen NN, Yu VSH, et al. Long-term success and survival of endodontic microsurgery. J Endod. 2020;46(2):149-157.e4. Link
-
Andreasen JO, Rud J. Correlation between histology and radiography in the assessment of healing after endodontic surgery. Int J Oral Surg. 1972;1(3):161-173. Link
-
Floratos S, Kim S. Modern endodontic microsurgery concepts. Dent Clin North Am. 2017;61(1):81-91. Link
-
Strbac GD, Schnappauf A, Giannis K, et al. Guided modern endodontic surgery: a novel approach for guided osteotomy and root resection. J Endod. 2017;43(3):496-501. Link
-
Setzer FC, Kratchman SI. Present status and future directions: surgical endodontics. Int Endod J. 2022;55(S4):1020-1058. Link
-
Liao WC, Lee YL, Tsai YL, et al. Outcome assessment of apical surgery: a study of 234 teeth. J Formos Med Assoc. 2019;118(6):1055-1061. Link
-
Khoury F, Hensher R. The bony lid approach for the apical root resection of lower molars. Int J Oral Maxillofac Surg. 1987;16(2):166-170. Link
-
Lee SM, Yu YH, Wang Y, et al. The application of “bone window” technique in endodontic microsurgery. J Endod. 2020;46(6):872-880. Link
-
Kim U, Kim S, Kim E. The application of “bone window technique” using piezoelectric saws and a CAD/CAM-guided surgical stent in endodontic microsurgery on a mandibular molar case. Restor Dent Endod. 2020;45(3):e27. Link
-
Hirsch V, Kohli MR, Kim S. Apicoectomy of maxillary anterior teeth through a piezoelectric bony-window osteotomy: two case reports introducing a new technique to preserve cortical bone. Restor Dent Endod. 2016;41(4):310. Link
-
Ahn SY, Kim NH, Kim S, et al. Computer-aided design/computer-aided manufacturing–guided endodontic surgery: guided osteotomy and apex localization in a mandibular molar with a thick buccal bone plate. J Endod. 2018;44(4):665-670. Link
-
Bello SA, Adeoye JA, Ighile N, Ikimi NU. Mental foramen size, position and symmetry in a multi-ethnic, urban black population: radiographic evidence. J Oral Maxillofac Res 2018;9(4):e2. Link
-
Abella F, de Ribot J, Doria G, et al. Applications of piezoelectric surgery in endodontic surgery: a literature review. J Endod. 2014;40(3):325-332. Link
-
Zhao R, Yang R, Cooper PR, et al. Bone grafts and substitutes in dentistry: a review of current trends and developments. Molecules. 2021;26(10):3007. Link
-
Floratos S, Molonis V, Tsolakis A, et al. Bone window technique in endodontic microsurgery – report of two cases. J Endod Microsurg. 2022;2:24-33. Link
-
Fan Y, Glickman GN, Umorin M, et al. A novel prefabricated grid for guided endodontic microsurgery. J Endod. 2019;45(5):606-610. Link
-
Ekici Ö, Aslantaş K, Kanık Ö, Keles A. Temperature and time variations during apical resection. Acta Odont Scand. 2021;79(2):156-160. Link
-
Bharathi J, Mittal S, Tewari S, et al. Effect of the piezoelectric device on intraoperative hemorrhage control and quality of life after endodontic microsurgery: a randomized clinical study. J Endod. 2021;47(7):1052-1060. Link